A 37-year-old healthy female patient with a prior history of laser-assisted in-situ keratomileusis (LASIK) in both eyes was referred to our clinic for help in managing her uncontrolled intraocular pressures (IOPs) in the setting of bilateral red eye, photophobia, and blurry vision. She had been managed by several ophthalmologists for 6 months prior to arriving for her visit. Her medical history was notable for sinusitis, for which she was given oral moxifloxacin shortly before the onset of her symptoms. At her initial visit with her primary ophthalmologist, she was noted to have IOPs of 30 mmHg in her right eye and 17 mmHg in her left eye, was diagnosed with bilateral hypertensive anterior uveitis, and was started on topical steroids and ocular hypertensives.
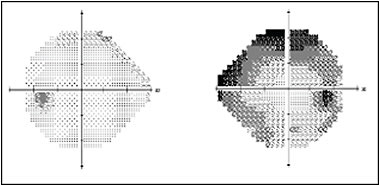
On arrival, the patient’s best-corrected vision was 20/60 and 20/20. Her right pupil was mydriatic and nonreactive with a right afferent pupillary defect by reverse. Her IOP was 28 mmHg in the right eye and 9 mmHg in the left eye on a regimen of latanoprost, brimonidine, dorzolamide-timolol (Cosopt), and oral methazolamide. She had a diffuse mild haze in both eyes and a paracentral stromal scar in the right eye within her LASIK flaps. The corneal findings were evaluated by a cornea specialist and were thought to be pressure-induced stromal keratitis from her initial pressure spike. There were trace pigmented cells in her right anterior chamber, and her left eye was quiet. The irides had diffuse patchy iris transillumination defects (TIDs) (Figure 1). On gonioscopy, she had open angles with heavy pigmentation of the trabecular meshwork. A moderate posterior subcapsular cataract was noted in the right eye. Fundus exam revealed small optic nerves with asymmetric cup-to-disc ratios of 0.6 in the right eye and 0.1 in the left eye. The nerve findings corresponded with the 24-2 Humphrey visual fields with significant changes in the right eye (Figure 2). Given the visually significant cataract and rapid glaucoma progression in the right eye, a combined cataract extraction and glaucoma procedure was indicated.

Solving the Mystery
The differential diagnoses for elevated IOP and iris pigmentary changes include trauma, pigment dispersion syndrome, pseudoexfoliation, herpetic uveitis, and Fuchs heterochromic iridocyclitis. Our patient underwent a full uveitis workup prior to her visit, which was negative for any infectious or autoimmune causes, and the clinical presentation did not fit the list of potential diagnoses.
Recently, a pair of interesting clinical entities, called bilateral acute depigmentation of the iris (BADI) and bilateral acute iris transillumination (BAIT), have been described.1,2 Both are female-predominant conditions characterized by severe bilateral photophobia, a pronounced pigmented anterior chamber reaction, and heavy pigmentation of the trabecular meshwork. Although the etiology is yet unknown, both conditions are female predominant, and a significant proportion of cases have been linked to upper respiratory infection with systemic fluoroquinolone use (particularly moxifloxacin) shortly before onset of symptoms. The 2 conditions can be distinguished from each other by their iris findings, effect on IOP, and clinical course. Bilateral acute depigmentation of the iris presents with depigmentation of the iris stroma, yielding a grayish, granular appearance.
In BADI, TIDs are typically absent, and BADI tends to have a milder clinical course with eventual resolution of iris changes and no significant effect on IOP. In contrast, the iris changes in BAIT are characterized by diffuse TIDs, mydriasis, and poor pupillary sphincter function. Intraocular pressure is often elevated and resistant to topical medications, often leading to oral carbonic anhydrase inhibitor use and surgical intervention. Our patient was diagnosed with BAIT given her severe pigmentary reaction with iris TIDs, treatment-resistant ocular hypertension IOP, and negative uveitis workup.
Surgical Approach and Outcome
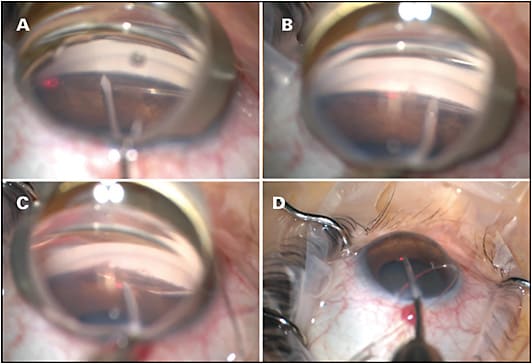
Our patient’s ocular hypertension was most likely due to pigment deposition and obstruction of the trabecular meshwork. Re-establishing aqueous outflow with a trabecular bypass procedure provided the most direct approach in reversing the pathology. Given her visually significant cataract and significantly elevated pressures despite maximal medical therapy, we decided on a combined cataract extraction and gonioscopy-assisted transluminal trabeculotomy (GATT). Under gonioscopic view, a nasal goniotomy was created using a microsurgical blade. A fiberoptic microcatheter (iTrack, Ellex iScience) was used to cannulate Schlemm’s canal. The microcatheter was advanced through the circumference of the canal using microforceps. The distal tip emerged from the nasal goniotomy and was grasped firmly. The proximal catheter was gently pulled to create a 360° trabeculotomy (Figure 3). Then, standard phacoemulsification cataract extraction and intraocular lens placement was performed. On postoperative day 1, her IOP improved to 12 mmHg off all medications. At her most recent follow-up at 8 months, she had a sustained reduction of IOP at 9 mmHg on dorzolamide-timolol.
Conclusion
Our patient presented with a severe pigmentary and inflammatory reaction resulting in glaucoma with IOP in the high 20s despite maximal medical therapy. While a filtering procedure would have otherwise been a reasonable choice, GATT allowed us to restore outflow through the conventional pathway by directly targeting the site of pathology. GP
References
- Yangzes S, Singh SR, Ram J. Bilateral acute depigmentation of iris. Indian J Ophthalmol. 2019;67(1):133.
- Tranos P, Lokovitis E, Masselos S, Kozeis N, Triantafylla M, Markomichelakis N. Bilateral acute iris transillumination following systemic administration of antibiotics. Eye (Lond). 2018;32(7):1190-1196.









