Glaucoma therapy, in the midst of the minimally invasive glaucoma revolution of the past several years, involves diligently treating the acute needs of each glaucoma patient with a keen eye on long-term planning for continued success. This mindset becomes even more critical in younger patients, as well as those with secondary and refractory glaucoma. A road map to success for these patients will likely involve multiple strategies aimed at different targets of the glaucoma treatment pathway over the course of their lives with the disease. It is these subsets of glaucoma that may see the greatest benefit of new approaches to glaucoma treatment. The evolution of surgical glaucoma treatment options may allow for the longevity of vision and improved lifestyle that was once only imagined.
Understanding the Terrain
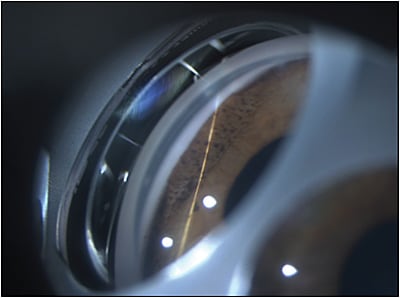
A 30-year-old female with iridocorneal endothelial syndrome (ICE) who had been followed for several years with elevated intraocular pressure (IOP) recently presented to my glaucoma clinic. She initially sought treatment 5 years ago with uncontrolled IOP in the high 30s and a Humphrey visual field with almost complete loss of the superior field and a 0.85 cup-to-disc ratio in the affected eye. Her corrected visual acuity at that time was 20/30. Her anterior-segment changes consisted of enlargement of her pupil with irregular endothelial appearance of the cornea. Gonioscopic examination revealed broad areas of peripheral anterior synechiae (Figure 1). After failure of multiple drop therapy, she was treated surgically with an Ahmed glaucoma implant (New World Medical). This initially lowered her IOP to the mid to high teens on 1 medication.
Unfortunately, over the course of several years, her IOP began to drift upward into the lower and mid 20s. There was a desire to avoid further surgical intervention due to her age and limited surgical options with her secondary glaucoma. Initial treatment involved adding multiple topical drops in an attempt to avoid the risks inherent with further surgery while lowering her risk of progression. At the height of her drop therapy, she was taking 5 different classes of topical medication to manage her disease.
Mapping a Course
As medications were added, the inevitability of issues with the ocular surface and therapy compliance increased. As irritation and redness became more of a problem, the IOP also began to rise back into the middle to high 20s with concern for progression on Humphrey visual field. A new interventional treatment was warranted. It is at this point in the care of a patient that glaucoma specialists have to consider the current surgical map and path options for glaucoma. Even at the time of this patient’s initial filtration surgery with an Ahmed shunt, her options were more linear. Many glaucoma treatment plans would simply be a straight line from diagnosis to medication or laser followed by filtration.
Our current course map allows for varied paths of travel. If our past option was only to take the highway to filtration, our current options involve a variance of scenic routes to reach our end goals of vision preservation through pressure control and consideration of patient lifestyle and goals. The main pathways fall into several categories, including treatment of trabecular or ciliary outflow, subconjunctival filtration through traditional or newer stenting procedures, and manipulation of aqueous flow through cyclodestruction.
Consider the patient when navigating a treatment path. In this case, due to the nature of the patient’s disease, which involved endothelial dysfunction and peripheral anterior synechiae within the angle, options for trabecular or ciliary outflow are eliminated. As recently illustrated, subconjunctival filtration with Xen (Allergan)1 or the Ex-Press shunt (Alcon)2 might be an option for this patient, despite her previous tube shunt. These devices may decrease the opportunity for proliferation of abnormal endothelial cells, which often cause failure of trabeculectomy in this disease.3 However, in this case, there was a desire to avoid the use of antifibrotics in a young female with an active lifestyle. These devices may remain viable options if needed in the future.
Finding Our Destination
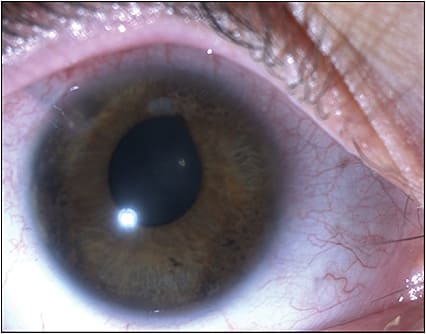
The decision was made to treat her glaucoma with micropulse transcleral diode laser cyclophotocoagulation. The Iridex Cyclo G6 laser was set at a micropulse power setting of 2,000 mW. Slow, sweeping 10-second movements were used to treat each of the 4 quadrants of the eye for a total of 60 seconds per quadrant (Figure 2). She was treated with a 3-week tapering dose of durezol starting at 3 times daily the first postoperative week. Her glaucoma medications were weaned over the course of the first 6 weeks after the procedure based on IOP. At her 6-month postoperative visit, her vision was 20/25 in the affected eye with an IOP of 8 mmHg on dorzolamide-timolol drops BID. She had also noted a decrease in ocular irritation and redness.
Micropulse transcleral diode laser cyclophotocoagulation is an effective treatment for refractory glaucoma and appears to have increased success in eyes with previous filtration surgery with relatively low complication rates.4,5 The case of this patient suggests that this procedure is also a viable alternative in the treatment of ICE-associated glaucoma. GP
References
- Lin MM, Morgan WH, Kolomeyer NN, et al. XEN gel stent to treat ICE syndrome: 4 cases. J Glaucoma. 2019;28(12):1090-1094.
- Colás-Tomás T, López Tizón E. Ex-PRESS mini-shunt implanted in a pregnant patient with iridocorneal endothelial syndrome. Eur J Ophthalmol. 2020;30(1):NP25-NP28.
- Chandran P, Rao HL, Mandal AK, Choudhari NS, Garudadri CS, Senthil S. Outcomes of primary trabeculectomy with mitomycin-c in glaucoma secondary to iridocorneal endothelial syndrome. J Glaucoma. 2016;25(7):e652-e656.
- Garcia GA, Nyugen CV, Yelinskiy A, et al. Micropulse transscleral diode laser cyclophotocoagulation in refractory glaucoma. Ophthalmol Glaucoma. 2019;2(6):402-412.
- Yelenskiy A, Gillette TB, Arosemena A, et al. Patient outcomes following micropulse transscleral cyclophotocoagulation: intermediate-term results. J Glaucoma. 2018;27(10):920-925.









