KDB Goniotomy Reduces IOP and Medication Burden
By Syril K. Dorairaj, MD
First introduced in 1930, goniotomy has long been considered a highly effective procedure for the treatment of congenital pediatric open-angle glaucoma. The emergence in 2015 of excisional goniotomy with the Kahook Dual Blade (KDB; New World Medical) introduced an evolved goniotomy procedure that considered the nuances in the pathology of adult glaucoma. The consequence is a procedure that reduces the intraocular pressure (IOP) and medication burden in a wide range of glaucoma patients.
The essential distinction between these 2 surgical techniques is that the original goniotomy is an incisional procedure, whereas KDB surgery is an excisional procedure that removes the trabecular meshwork (TM). The traditional goniotomy knife is used to produce a single incision in the TM, does not remove TM tissue, and has the potential to injure the sclera.1 Conversely, the single-use KDB ophthalmic instrument is designed to remove the TM with minimal residual TM leaflets and less collateral damage.
Goniotomy with the KDB addresses the primary cause of elevated IOP by removing the obstruction to aqueous outflow at the level of the diseased TM. The KDB has a distal tip that pierces the TM, enters Schlemm’s canal, and then elevates, stretches, and uses 2 parallel blades to excise a full strip of TM. This process re-establishes the normal flow of aqueous into Schlemm’s canal and the distal collector channels, accomplishing this goal without the formation of a bleb, thereby avoiding potential bleb-related complications.2 This procedure also avoids the implantation of a permanent device, which in turn negates the possibility of erosion, migration, or endothelial cell loss. In my experience and in the literature, excisional goniotomy with the KDB effectively and safely lowers IOP and the need for IOP-lowering medications, and the amount of IOP reduction meets or exceeds the recommended targets for most patients with glaucoma.3-5
Anecdotal and Clinical Evidence
When I started performing KDB goniotomy, I offered it as a combined option for patients who were undergoing cataract surgery and had mild-to-moderate glaucoma. Over time, I noticed that these patients were faring better than expected: medications were reduced to 1 or none; there were few complications, and these medications were easily resolved; and patients’ glaucoma was increasingly stable over time. These results were so encouraging that we began offering the procedure to a wider swath of patients.
Today, a growing body of evidence — including several multicenter studies — supports the efficacy and safety of KDB goniotomy across all glaucoma severities, either as a stand-alone procedure or in conjunction with cataract surgery, for primary open-angle glaucoma, as well as in conjunction with goniosynechialysis and phacoemulsification for angle-closure glaucoma (ACG) (Table 1).
| Author | Design | Severity | No. Eyes | Study Duration | Baseline IOP (mmHg) | Mean IOP Reduction (mmHg) | Mean Endpoint IOP (mmHg) | IOP Change | Mean Medication Change | Eyes ≥20% IOP Reduction | Eyes ≥1 Medication Reduction | Eyes Medication Free at Endpoint | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Excisional goniotomy with cataract surgery | |||||||||||||
| Greenwood et al7 | Prospective | Mild-moderate-severe | 71 | 6 mo. | 17.4 | -4.6 | 12.8 | -26% | -0.7 | 58.3% | 61.7% | – | |
| Dorairaj et al16 | Prospective | Mild-moderate-severe | 52 | 12 mo. | 16.8 | -4.4 | 12.4 | -26% | -0.8 | 57.7% | 63.5% | – | |
| Dorairaj et al22 | Retrospective (iStent comparator) | Mild-moderate | 237 | 6 mo. | KDB 17.9 | -4.2 | 13.7 | -23.7% | -1.1 | 56.1% | 77.6% | 59% | |
| 198 | iStent 16.7 | -2.7 | 14.0 | -16.4% | -0.9 | 43.9% | 64.1% | 43% | |||||
| ElMallah et al23 | Retrospective (iStent comparator) | Mild-moderate | 190 | 12 mo. | KDB 18.2 | -5.0 | 13.2 | -27.5% | -1.03 | 64.2% | 80.4% | – | |
| 125 | iStent 16.7 | -2.3 | 14.4 | -13.7% | -0.97 | 41.6% | 77.4% | – | |||||
| Sieck et al9 | Retrospective | Mild-moderate-severe | 165 | 12 mo. | 16.7 | -2.9 | 13.8 | -17.3% | -0.4 | – | – | – | |
| Hirabayashi et al19 | Retrospective | Severe | 42 | 6 mo. | 17.1 | -2.1 | 15.0 | -12.3% | -1.2 | – | – | 31% | |
| Dorairaj et al24 | Retrospective | Angle closure (goniosynechialysis + goniotomy) | 42 | 6 mo. | 25.5 | -12.7 | 12.8 | -48.8% | -2.2 | 100% | 100% | 86% | |
| Dorairaj et al11 | Retrospective | Angle closure (goniosynechialysis + goniotomy) | 42 | 12 mo. | 25.5 | -12.3 | 13.3 | -47.2% | -2.2 | 100% | 95% | 86% | |
| Stand-alone excisional goniotomy | |||||||||||||
| Sieck et al9 | Retrospective | Mild-moderate-severe | 32 | 12 mo. | 20.4 | -6.3 | 14.1 | -31% | -0.8 | – | – | – | |
| Berdahl et al25 | Retrospective | Mild-moderate-severe | 53 | 6 mo. | 23.5 | -8.5 | 15.0 | -36.2% | -1.0 | 69.8% | 67.9% | – | |
| Salinas et al21 | Retrospective | Severe/refractory | 53 | 6 mo. | 18.4 | -4.4 | 14.0 | -23.9% | -1.2 | 57.7% | 63.3% | – | |
| KDB medians | 18.2 | -4.6 | 13.7 | -26% | -1.1 | ||||||||
An overview of early study outcomes illustrates its efficacy and safety.
A multicenter study of 71 eyes that underwent phacoemulsification in combination with KDB showed an IOP drop of 28% at 1 year. The preoperative IOP average in this study was 17.4 mmHg, and the 1-year postoperative IOP was 12.5 mmHg. The same cohort had 64% of patients with at least 1 medication reduction.6
In another multicenter study, 58.3% of patients had an IOP reduction of at least 20%, and 61.7% were using at least 1 fewer IOP-lowering medication after 6 months of follow-up.7
A retrospective review of adult patients who underwent goniotomy either with or without phacoemulsification showed a significant decrease in IOP of 5.8 mmHg from baseline in the KDB stand-alone group and 4.7 mmHg in the phaco-KDB cohort. IOP-lowering medications were also significantly reduced by 0.8 and 0.7 medications, respectively, at 6 months of follow-up.8
A retrospective review of 180 eyes that underwent either KDB goniotomy alone or KDB combined with phacoemulsification showed a significant decrease in IOP and medication usage at 1 year, with success defined as at least a 20% decrease in IOP, which was achieved in approximately 70% of patients who underwent phaco-KDB and in approximately 67% of patients who underwent KDB alone.9
Long-Term Outcomes
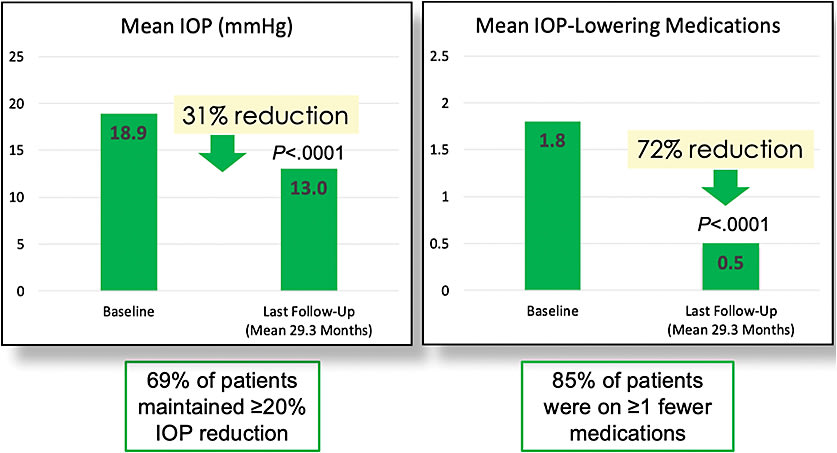
Until recently, however, substantive long-term results had been lacking. Recently, approximately 3 years of follow-up were reported of the earliest patients undergoing KDB excisional goniotomy in combination with cataract surgery in our study. This follow-up is the longest available of combined excisional goniotomy-phacoemulsification: 26 patients were followed for a mean of 29.3 months (range 22-35 months) after combined surgery. From a mean baseline IOP of 18.9 mmHg, the mean IOP at the last follow-up was 13.0 mmHg, representing a 31% reduction. IOP-lowering medications were reduced from a mean of 1.8 medications at baseline to 0.5 medications at the last follow-up, representing a 72% reduction. Ultimately, 69% of patients had IOP reductions greater than 20% from baseline, and 85% were on at least 1 fewer medication (Figure 1). These patients have experienced a minimum of 3 years of life without eye drops, which is quite significant. I stress the importance of patients returning every 6 months to monitor their disease. So far, these 3-year data are very promising.10
Aggressive Angle-Closure Glaucoma
There have also been positive outcomes with KDB in ACG patients. Angle-closure glaucoma can be very aggressive, but if it is detected early and treated promptly, progression and vision loss can be stopped. Success in treating this aggressive form of glaucoma has been both surprising and fulfilling. Goniotomy using KDB and KDB-assisted goniosynechialysis combined with phacoemulsification allow for the aqueous humor drainage pathway to be re-established through disruption of the peripheral anterior synechiae and removal of part of the dysfunctional TM.
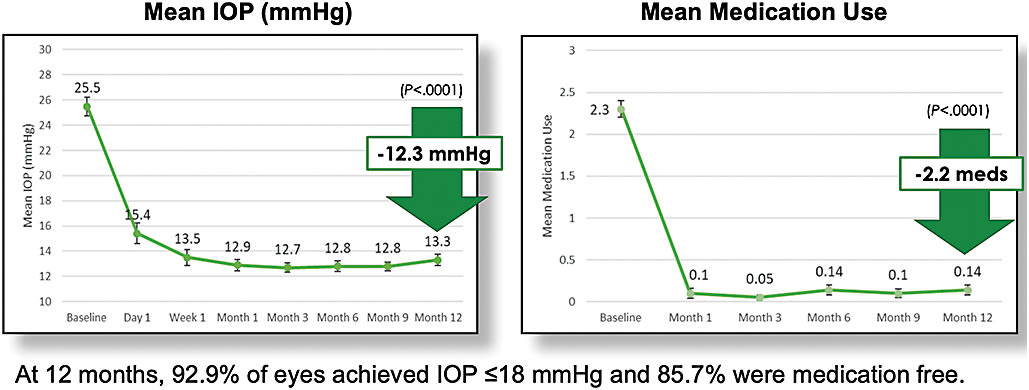
In a retrospective, interventional case series of 42 eyes of 24 patients with ACG and cataracts, IOP was reduced by 47.2% from a baseline of 25.5 mmHg to 13.3 mmHg at 12 months, and 92.9% of eyes achieved IOP of 18 mmHg or lower. Medication burden was reduced by a mean of 2.2 medications from 2.3 at baseline to 0.5 at 12 months, and 85.7% of patients were medication free (Figure 2).11
To ensure success with this combination of procedures for ACG, it is important to perform a thorough preoperative and postoperative exam by gonioscopy and computed tomography imaging to monitor for the development of peripheral anterior synechiae. I recommend that surgeons first refine and become competent with their KDB goniotomy techniques for open-angle patients and then introduce it to angle-closure patients. Performing this combination of procedures in this patient population affords a sense of accomplishment because the disease essentially stops. This option is safer than alternative surgical procedures that may have a higher rate of complications.12
Conclusion
In general, excisional goniotomy offers faster recovery and the opportunity to treat all levels of glaucoma severity surgically. The primary benefit of using a KDB is its precision and its ability to significantly lower IOP. In some cases, it can halt disease progression (such as with ACG). It can also reduce or completely stop eye drop use, which reduces long-term medication-associated toxicity and well-known medication adherence challenges.
KDB Goniotomy Helps Reshape the Glaucoma Surgery Paradigm
By Jella An, MD
Compared to alternative interventions, such as pharmaceuticals or laser treatment, glaucoma surgery was long considered the most direct route to the greatest amount of IOP reduction.12 Surgery was, however, often left as a last resort for refractory disease due to its high rate of complications and long-term risk of bleb-related problems.
Since the advent of minimally invasive glaucoma surgery (MIGS), the paradigm is shifting. MIGS is a safe and effective treatment option that can be implemented earlier in the course of disease and may reduce morbidity due to progression, thus preventing or delaying the need for filtering or shunt surgeries.13,14 MIGS has grown from a single procedure to an entire category, encompassing a broad spectrum of surgical choices that can be personalized to each patient’s needs, risk profile, and treatment target. Moreover, for patients with coexisting glaucoma and cataracts, MIGS has expanded the range of options available for surgical comanagement of these conditions.
Goniotomy With KDB
Unlike traditional goniotomy, which is often performed in congenital glaucoma, the KDB’s unique design allows for complete resection of diseased TM on the inner wall of Schlemm’s canal, facilitating continuous flow of aqueous humor from the anterior chamber to the collector channel and distal pathway outflow system15 A step-by-step video guide to KDB goniotomy (ab-interno trabeculectomy; Figure 3) combined with phacoemulsification is available at youtu.be/XhYyCySUKdc . The sidebar presents some clinical pearls for surgery.

SURGICAL PEARLS FOR KDB PROCEDURE
- Start with a cooperative patient with a clear view of the angle.
- Use light sedation.
- Avoid cutting the limbal vasculature.
- Use a 2.0-mm flared incision to start.
- Try a goniostabilizer for globe control.
- Use cohesive viscoelastics to keep the chamber formed.
- Stay in the canal with heel to wall to ensure parallel trabecular meshwork incisions.
- Aim for the largest degree of incision, and completely remove the resected trabecular meshwork with microforceps.
- An outside-in technique (2 clock hours clockwise, then 2 clock hours counterclockwise incision) often prevents the need for forceps to pull out the excised trabecular meshwork strip.
Patient Selection
Careful patient selection is integral to achieving optimal outcomes with MIGS. Classic indications for MIGS are mild to moderate open angle glaucoma in patients who have visually significant cataracts and are on multiple medications. What is equally or perhaps even more important, however, is the target IOP — factoring in the patient age, rate of disease progression, and other comorbidities.
The best candidates for goniotomy with KDB are those who are cooperative, will benefit from enhanced aqueous outflow, and have a pigmented nasal TM with clear anatomy that offers a good view on gonioscopy. Conversely, patients are contraindicated for goniotomy with TM excision who have active neovascular disease, active uveitic glaucoma, elevated episcleral venous pressure, poor view of the angle, and a goal IOP lower than the mid-teens. Ultimately, any glaucoma patients who require incisional management of their disease or are also undergoing cataract surgery may be considered for this procedure.
Clinical Study Data
Throughout the 3.5 years that I have been performing this procedure, I have found it to be extremely safe, with both a short learning curve of approximately 10 cases and an operating time of roughly 5 minutes in addition to cataract surgery. Since the introduction of the KDB in 2015, a growing number of studies have demonstrated its efficacy and safety in reducing IOP and medication burden.16,17 For instance, in a recent study comparing the outcomes of 360° circumferential trabeculotomy vs sectoral goniotomy with the KDB, we found that, while both KDB and Trab360 (Sight Sciences) or gonioscopy-assisted transluminal trabeculectomy procedures similarly lowered IOP and the need for IOP-lowering medications during the first 6 postoperative months, more eyes undergoing KDB excisional goniotomy than 360° trabeculotomy attained target IOP ≤18 mmHg and ≤15 mmHg at 6 months.18 In this study, we examined 74 eyes of 61 patients with primary open-angle glaucoma of all stages, with more than half of them being severe. Approximately 82% of patients achieved a 20% IOP reduction or a medication reduction from baseline without an additional glaucoma procedure 6 months postoperatively. Our results suggest that removal of the full 360° TM may not be necessary to achieve desirable surgical outcomes in adult patients with glaucoma when combined with cataract surgery.
These findings support the observation that more is not always better and that 90° sectoral goniotomy using KDB may be equivalent or superior to a 360° circumferential trabeculotomy using a suture method. Whether this outcome occurs because there is a point of diminishing returns with the degree of TM bypass or due to the different methods of bypass (excision vs incision of TM) is not yet known. Among the things that are known are that it is important to completely remove the strip of TM resected with KDB from the angle because the stump of TM left behind can be a nidus for postoperative closure.
With excisional goniotomy with KDB, most patients achieve IOP in the mid-teens regardless of baseline IOP. Patients who have mild glaucoma and are on fewer medications tend to have better results, but many severe glaucoma patients also achieve excellent results. Another recent study reflects these outcomes.19 We studied 42 eyes from 36 patients with severe open angle glaucoma (“severe” per ICD-10 grading) who underwent phaco-KDB. At 6 months, 64.3% (27/42) of eyes had achieved IOP ≤15 mmHg without additional glaucoma procedures; 45.2% (19/42) reached this target IOP on fewer medications and 31.0% (13/42) on no medications.
In another recent study, we compared the surgical outcomes between excisional goniotomy using the KDB and the iStent (Glaukos) in combination with phacoemulsification and found that both provided comparable IOP and medication reductions. However, the proportion of eyes able to discontinue 1 or more medications while maintaining IOP ≤18 mmHg was significantly greater in eyes undergoing KDB.20
The most common complications are IOP spikes secondary to steroid response and early postoperative blood reflux that is generally transient.21 Repeat bleeds are rare, unless the eye becomes hypotonous below episcleral venous pressure. For example, we do see reflux heme even several months after surgery with compression gonioscopy when the IOP is close to episcleral venous pressure. However, spontaneous and clinically significant bleeds after the 2-week mark are extremely rare.
Conclusion
In addition to providing a surgical alternative that can be implemented earlier in the course of disease and can prevent or delay more invasive filtering procedures, excisional ab-interno trabeculectomy with KDB provides a cost-effective method for performing goniotomy with a proven CPT code: 65820. This ability means that you can use KDB in a variety of glaucoma patients and conditions, including angle closure and secondary glaucoma, as a stand-alone or combined procedure. GP
References
- Francis BA, Akil H, Bert BB. Ab interno Schlemm’s canal surgery. Dev Ophthalmol. 2017;59:127-146.
- Zahid S, Musch DC, Niziol LM, Lichter PR; Collaborative Initial Glaucoma Treatment Study Group. Risk of endophthalmitis and other long-term complications of trabeculectomy in the Collaborative Initial Glaucoma Treatment Study (CIGTS). Am J Ophthalmol. 2013;155(4):674-680.
- Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Collaborative Normal-Tension Glaucoma Study Group. Am J Ophthalmol. 1998;126(4):487-497.
- American Academy of Ophthalmology. Primary open-angle glaucoma: preferred practice pattern. San Francisco, CA: American Academy of Ophthalmology; 2015.
- European Glaucoma Society. Terminology and Guidelines for Glaucoma. 4th ed. Savona, Italy: PubliComm; 2014.
- Mansouri K, Radcliffe N, Lazcano G, et al. Intraocular pressure reduction after use of a novel goniotomy blade combined with phacoemulsification. Poster presented at: 7th World Glaucoma Congress; June 21-July 1, 2017; Helsinki, Finland.
- Greenwood MD, Seibold LK, Radcliffe NM, et al. Goniotomy with a single-use dual blade: Short-term results. J Cataract Refract Surg. 2017;43(9):1197-1201.
- Radcliffe N, Abdullah S, Jasek M, et al. A novel dual blade device for goniotomy: Six-month follow-up. Poster presented at: 27th Annual Meeting of the American Glaucoma Society; March 2-5, 2017; Coronado, CA.
- Sieck EG, Epstein RS, Kennedy JB, et al. Outcomes of Kahook dual blade goniotomy with and without phacoemulsification cataract extraction. Ophthalmol Glauc. 2018;1(1)75-81.
- Dorairaj S, et al. Prospective long-term efficacy outcomes of excisional goniotomy with the Kahook dual blade combined with cataract surgery. Poster presented at: Annual Meeting of the American Society of Cataract and Refractive Surgery; May 3-7, 2019; San Diego, CA.
- Dorairaj S, Tam MD, Balasubramani GK. Twelve-month outcomes of excisional goniotomy using the Kahook Dual Blade in eyes with angle-closure glaucoma. Clin Ophthalmol. 2019;13:1779-1785.
- Lichter P, Musch D, Gillespie B, et al. Interim clinical outcomes in the collaborative initial glaucoma treatment study comparing initial treatment randomized to medications or surgery. Ophthalmology. 2001;108(11):1943-1953.
- Pillunat L, Erb C, Jünemann A, Kimmich F. Micro-invasive glaucoma surgery (MIGS): a review of surgical procedures using stents. Clin Ophthalmol. 2017;11:1583-1600.
- Chen DZ, Sng CCA. Safety and efficacy of microinvasive glaucoma surgery. J Ophthalmol. 2017;2017:3182934.
- Seibold L, Soohoo JR, Ammar DA, Kahook MY. Preclinical investigation of ab interno trabeculectomy using a novel dual-blade device. Am J Ophthalmol. 2013;155(3):524-529.
- Dorairaj S, Seibold L, Radcliffe N, et al. 12-month outcomes of goniotomy performed using the kahook dual blade combined with cataract surgery in eyes with medically treated glaucoma. Adv Ther. 2018;35(9):1460-1469.
- Greenwood M, Seibold L, Radcliffe N, et al. Goniotomy with a single-use dual blade: short-term results. J Cataract Refract Surg. 2017;43(9):1197-1201.
- Hirabayashi MT, Lee D, King JT, Thomsen S, An JA. Comparison of surgical outcomes of 360° circumferential trabeculotomy versus sectoral excisional goniotomy with the Kahook Dual Blade at 6 months. Clin Ophthalmol. 2019;13:2017-2024.
- Hirabayashi MT, King JT, Lee D, An JA. Outcome of phacoemulsification combined with excisional goniotomy using the Kahook Dual Blade in severe glaucoma patients at 6 months. Clin Ophthalmol. 2019;13:715-721.
- Lee D, King J, Thomsen S, Hirabayashi M, An J. Comparison of surgical outcomes between excisional goniotomy using the Kahook Dual Blade and iStent trabecular micro-bypass stent in combination with phacoemulsification. Clin Ophthalmol. 2019;13:2097-2102.
- Salinas L, Chaudhary A, Berdahl J, et al. Goniotomy using the Kahook Dual Blade in severe and refractory glaucoma: six month outcomes. J Glaucoma. 2018;27(10):849-855.
- Dorairaj SK, Kahook MY, Williamson BK, Seibold LK, ElMallah MK, Singh IP. A multicenter retrospective comparison of goniotomy versus trabecular bypass device implantation in glaucoma patients undergoing cataract extraction. Clin Ophthalmol. 2018;12:791-797.
- ElMallah MK, Seibold LK, Kahook MY, Williamson BK, Singh IP, Dorairaj SK; KDB Goniotomy Study Group. 12-month retrospective comparison of Kahook Dual Blade excisional goniotomy with iStent trabecular bypass device implantation in glaucomatous eyes at the time of cataract surgery. Adv Ther. 2019;36(9):2515-2527.
- Dorairaj S, Tam MD. Kahook Dual Blade excisional goniotomy and goniosynechialysis combined with phacoemulsification for angle-closure glaucoma: 6-month results. J Glaucoma. 2019;28(7):643-646.
- Berdahl JP, Gallardo MJ, ElMallah MK, et al. Six-month outcomes of goniotomy performed with the Kahook Dual Blade as a stand-alone glaucoma procedure. Adv Ther. 2018;35:2093-2102.










