Glaucoma can be broadly classified as either open angle or closed angle. The closed form is known as angle-closure glaucoma and can be primary without a known cause, or secondary. Primary angle closure has known contributing factors that lead to the iris appositionally or synechially obstructing outflow through the trabecular meshwork.
The 2 main causes of primary angle closure are pupillary block, in which there is apposition of the lens and iris causing more peripheral apposition, and plateau iris syndrome (PIS), in which there is direct apposition of the iris and trabecular meshwork. In pupillary block, contact between the iris and the lens impedes the flow of aqueous from the posterior chamber to the anterior chamber, resulting in higher pressure behind the iris than in front. This pressure gradient then pushes the iris anteriorly against the trabecular meshwork. In plateau iris, the ciliary body is rotated anteriorly, pushing the iris against the trabecular meshwork, resulting in the same outcome. These 2 mechanisms may often coexist.
Differentiating the mechanism of angle closure is essential to planning the correct treatment. Angle closure due to pupillary block can be relieved by laser iridotomy, but this is an ineffective treatment for plateau iris configuration. Laser iridotomy may have some treatment effect in combined mechanism cases.
Identifying Etiology
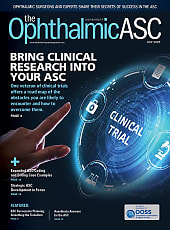
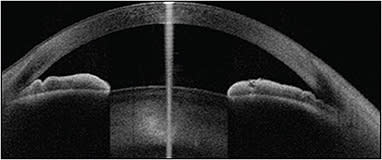
Anterior-segment optical coherence tomography and ultrasound biomicroscopy are both valuable in determining underlying etiology in a patient with angle closure. Pupillary block can be seen clinically as iris bowing (Figure 1), with visible space between the midperipheral iris and the lens due to the higher pressure behind the iris. In contrast, plateau iris configuration results in a steep peripheral angle and a deeper central anterior chamber.1 On gonioscopy, a “double hump sign” can be seen with a peripheral iris hump created by the ciliary body pushing on the iris root and a central hump caused by the rest of the iris sitting on the surface of the lens.2 On ultrasound biomicroscopy, there will be a lack of a ciliary sulcus and likely flattening of the ciliary muscle (Figure 2).
Plateau iris syndrome was first described in 1958, and the syndrome was further elucidated in 1977 after several failed peripheral iridotomies occurred with angle closure despite deep anterior chambers.3 The average age at presentation for PIS is approximately 34 years, with a predilection for (73% of cases) mild to moderate hyperopic women.4,5 Although it is multifactorial, there appears to be a hereditary component to PIS, and screening should, therefore, be tailored toward younger patients and their family members.6 It is discovered on eye exams of patients complaining of intermittent headaches previously misdiagnosed as migraines.
Historically, PIS has been treated with argon laser peripheral iridoplasty to burn and contract the peripheral iris root to widen the angle.3 However, the angle is still prone to closing after this procedure, and risks include pupillary abnormalities, iris ischemia, or even iridodialysis during routine cataract surgery.7 More recently, lens extraction has become the treatment of choice in many cases of angle closure, even in cases with a clear lens. However, while lens extraction is very effective in relieving and preventing future pupillary block, it does not always open the angle adequately in cases of PIS, because it does not reposition the ciliary body. Additional treatment may be required to ensure the desired outcome.
Endoscopic Cycloplasty
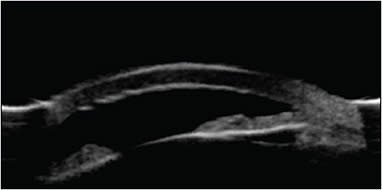
Endoscopic cycloplasty (ECPL; BVI), or endocycloplasty, is a treatment that ablates the posterior ciliary processes under direct endoscopic visualization.8 In this procedure, a diode laser is applied to the posterior aspect of the ciliary processes. The energy discharged to the tissue causes a thermal reaction creating tissue contraction, which rotates the ciliary processes posteriorly. After application, the angle becomes wider and the peripheral iris flatter (Figure 3).
Endocycloplasty can easily be performed in conjunction with lens extraction. Once the lens has been removed, ECPL is best performed over 120° to 160°, opposite the main incision for lens extraction. As the laser microendoscope is passed through the wound and underneath the nasal iris, the probe is aimed posteriorly and deep between the ciliary processes. Treatments greater than 160° are often not necessary, because only a portion of the angle needs to be open to avoid future issues. Energy should be titrated higher as needed to produce a visible shrinking effect and posterior rotation. Postoperative management is straightforward and similar to lens extraction alone. However, more frequent dosing of topical corticosteroids may be required.
In a recent study of 23 eyes with PIS, 10 (43%) underwent combined lens extraction with endocycloplasty (LE/ECPL), and 13 (57%) received lens extraction (LE) alone.9 After treatment, angles were significantly deepened in both groups (P<.001). Changes in angle opening distance, trabecular-iris space area, and trabecular-iris circumference volume from pretreatment to post-treatment showed that the magnitude of deepening in treated (nasal) quadrants was greater in LE/ECPL eyes than in eyes undergoing LE alone (P<.05). Within the LE/ECPL group, the ECPL-treated angles were deepened more than the untreated angles by all 3 parameters (P<.002). These data suggest that a combined approach is more effective at opening the angle compared to standalone LE, without compromising the safety profile. Typically, it is my personal practice to perform phacoemulsification/ECPL on PIS patients in the first eye. If only the nasal angle opens adequately, I will perform the same combined procedure in the second eye. If there is adequate opening in the untreated portion of the angle, then I will perform phacoemulsification alone in the second eye.
Endocycloplasty is a promising new treatment modality for PIS. Although further longitudinal studies are necessary, initial data demonstrate a strong safety profile and convincing efficacy. GP
References
- Kumar RS, Baskaran M, Chew PT, et al. Prevalence of plateau iris in primary angle closure suspects an ultrasound biomicroscopy study. Ophthalmology. Mar 2008;115(3):430-434.
- Desai, M. Plateau iris. Available at: https://eyewiki.aao.org/Plateau_Iris#cite_note-Filho-1 . Accessed January 10, 2020.
- Diniz Filho A, Cronemberger S, Merula RV, Calixto N. Plateau iris. Arq Bras Oftalmol. 2008;71(5):752-758.
- Stefan C, Iliescu DA, Batras M, Timaru CM, De Simone A. Plateau iris--diagnosis and treatment. Rom J Ophthalmol. 2015;59(1):14-18.
- Ritch R, Chang B, Liebmann J. Angle closure in younger patients. Ophthalmology. 2003;110(10):1880-1889.
- Ahram DF, Alward WL, Kuehn MH. The genetic mechanisms of primary angle closure glaucoma. Eye (Lond). 2015;29(10):1251-1259.
- Wang JC, Lee PS, Ritch R. Plateau iris glaucoma. May 6, 2016. Available at: http://emedicine.medscape.com/article/1207281-overview . Accessed January 10, 2020.
- Uram M. Ophthalmic laser microendoscope ciliary process ablation in the management of neovascular glaucoma. Ophthalmology. 1992;99(12):1823-1828.
- Lu M, Chuang AZ, Feldman RM. Comparing the effect of lens extraction with endocycloplasty and lens extraction alone on peripheral angle anatomy in eyes with plateau iris configuration. Paper presented at: AGS Annual Meeting; San Francisco, California; March 2019.