As the list of minimally invasive glaucoma surgeries (MIGS) has grown and evolved over the last few years, the Xen gel stent (Allergan) continues to be an effective treatment for glaucoma patients. It enables glaucoma surgeons to achieve substantial reductions in intraocular pressure (IOP) while minimizing vision-threatening complications.
Implantation of the Xen gel stent is unique in that there are multiple options: open conjunctiva, closed conjunctiva, ab interno, and ab externo. Surgeons who use Xen may vary their technique depending on the patient profile, but in our respective practices, we tend to stick to a preferred technique in most cases.
Dr. Panarelli: Open Conjunctiva
Choosing This Approach
The techniques for Xen implantation are evolving, and I think we will learn more about when to use each of the approaches in different situations. Today I use an ab-externo open-conjunctiva approach in almost all cases. Certainly, it’s the better choice for patients with prior incisional surgery who might have challenging anatomy or higher risk for scarring. In these “high-risk” cases, I prefer to open the tissue, dissect a pocket, and apply a higher dose of mitomycin C. I reserve closed-conjunctiva implantation for very deep-set eyes with prominent brows or for older patients who have very little Tenon tissue.
One reason for my choice is reproducibility. When I place the device beneath the Tenon layer, the results are so reproducible that challenging cases take the same amount of time as easier ones. In my practice, I also see better outcomes and bleb appearance compared to the closed conjunctiva approach.
Another advantage is that the open-conjunctiva technique can be taught very easily. The technique is a hybrid between a trabeculectomy and a tube shunt surgery, with the potential for similar efficacy and a better safety profile.1 The way we handle the tissue is akin to trabeculectomy, and the needle track and insertion are similar to some steps in tube shunt surgery. Surgeons who have performed traditional glaucoma surgeries can lean on their experience and master the Xen open-conjunctiva technique after just a handful of cases.
The Open-conjunctiva Technique
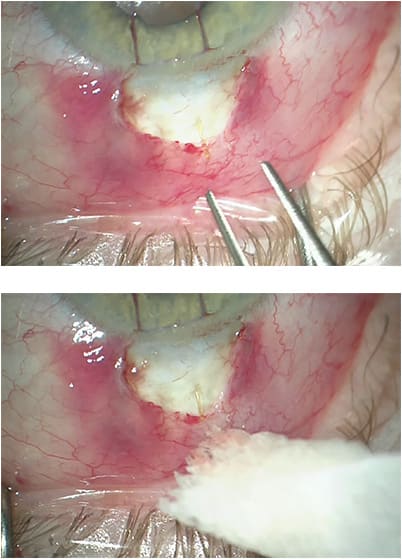
I begin by injecting 60 µg of mitomycin C into the subconjunctival/sub-Tenon space about 10 mm posterior to the limbus (0.15 mL of a 0.4 mg/mL concentration).2 Using a fornix-based approach, I make a 3 o’clock conjunctival peritomy at the limbus. I dissect and create a pocket in either the superionasal or the superiotemporal quadrant with Westcott tenotomy scissors and apply gentle cautery to the area.
Next, using a 27-gauge bent needle, I make a 2-mm tunnel track into the anterior chamber. For certain highly myopic patients or patients whose sclera is thin, I use a 30-gauge needle. I remove the Xen gel stent from the inserter and use nontoothed forceps to slide it into the track that I’ve just created.
Finally, I confirm flow through the distal end by “priming” the device. I fill the anterior chamber above a physiologic pressure, and then I wait to see percolation of fluid through the distal end of the stent. Once I’ve seen that, I bring the conjunctiva and Tenon up to the limbus and close the incisions in a watertight fashion (Figure 1).
Dr. Grover: Closed Conjunctiva
Choosing This Approach
When Xen was first approved, I used solely the ab-interno approach for about a year and a half. When I learned about the ab-externo method at an American Academy of Ophthalmology meeting, I began to try that technique. My colleagues and I evaluated the data retrospectively and found that the results and recovery for ab-interno and ab-externo implantation have been very similar. It’s important for glaucoma specialists to learn and feel comfortable with both techniques, because we need to meet the needs of various patients, depending on anatomy and other features of their eye.
Today, I choose the ab-interno technique for implanting Xen combined with cataract surgery, because I’m already inside the eye. I also choose ab-interno implantation for patients whose conjunctivas are very frail and can’t be moved because the ab-externo approach requires me to pinch and mobilize the conjunctiva. When we use Xen as a stand-alone procedure, it’s nice to inject the device ab-externo without incising the conjunctiva and without having to make a corneal incision. It’s also a much more efficient approach if you don’t have to go into the eye, and it allows us to treat patients with very prominent cheekbones.
The Closed-conjunctiva Technique
Using traction sutures in the cornea, I rotate the eye down and use calipers to mark 2.5 mm posterior to the limbus. My scleral tunnel is always a little bit shorter than I plan it to be, so if I aim for 2.5 mm, my scleral tunnel in fact is usually 2 mm.
Next, I pinch the conjunctiva in the superiotemporal quadrant and pull it down in the inferior nasal quadrant. With my other hand, I enter the anterior chamber through a scleral tunnel approaching 2.5 mm posteriorly to the limbus at around the 12 o’clock position. I pinch and drag the conjunctiva so that the small conjunctival opening is away from where the Xen will lie. If the conjunctival opening is next to the Xen, there is greater risk for a conjunctival buttonhole and a leak — and possibly an erosion.
My goal for implanting Xen is for it to enter the anterior chamber just anteriorly to the trabecular meshwork and make it as parallel as possible to the iris. With the 6-mm implant, the ideal proportions are 1 mm in the anterior chamber, 2 mm in the sclera, and 3 mm in the subconjunctival space.
Using the traction suture, I rotate the globe inferiorly as I manipulate the conjunctiva and prepare to pass the injector into the conjunctiva. As I enter the anterior chamber, I pull the traction suture a little superiorly for countertraction as I get into the eye. Once I can see the needle bevel in the anterior chamber, I confirm I am in good position. As I inject the implant and slide the injector anteriorly, the Xen is inserted into the anterior chamber. Once the Xen is injected, the needle starts to retract, as I continue to slide the injector anteriorly. When the needle disengages the wall of the eye, there is a very high risk of a flick. To avoid this, I pull inferiorly and anteriorly on the traction suture, which allows me to remain in complete control of the globe, thus minimizing the risk of flick (Figure 2).
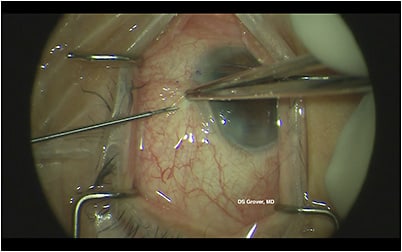
Finally, I verify using gonioscopy that the Xen is in good position, with adequate proportions in the anterior chamber, sclera, and subconjunctival space. The subconjunctival portion of the Xen can be manipulated if fine tuning of the position is needed. GP
References
- Schlenker MB, Gulamhusein H, Conrad-Hengerer I, et al. Efficacy, safety, and risk factors for failure of standalone ab interno gelatin microstent implantation versus standalone trabeculectomy. Ophthalmology. 2017;124(11):1579-1588. doi:10.1016/j.ophtha.2017.05.004
- Panarelli JF, Yan DB, Francis B, Craven ER. XEN Gel Stent open conjunctiva technique: a practical approach paper. Adv Ther. 2020;37(5):2538-2549. doi:10.1007/s12325-020-01278-1










