Intraocular pressure (IOP), currently the only known modifiable risk factor for glaucoma treatment, has a definite circadian rhythm, and numerous studies have confirmed that fluctuation of IOP can lead to the worsening of glaucoma-related damage. Because glaucoma patients come to the clinic only once every several months for follow-up appointments, and many times prefer to come in during the same time of day each visit, identifying fluctuations in IOP that would prompt disease management changes is challenging. This article discusses the subset of glaucoma patients who can benefit from remote IOP monitoring, and the future of remote IOP monitoring.
Diurnal IOP checks are not a new concept, but the major limitation has been that patients are only present during routine office hours. Newer technologies now allow us to obtain 24-hour readings over a span of several days. The question that we need to answer, though, is whether more data are always helpful and to what extent they influence decision making. Home monitoring may actually obtain more information than we need in some cases. A patient’s glaucoma can be well controlled with no structural changes over time, yet they can have IOPs outside of the target range on certain days. A glaucoma specialist might not intervene for each elevated IOP in cases such as this, whereas an ophthalmologist who hasn’t garnered a nuanced understanding of glaucoma might treat unnecessarily.
Applications for Diurnal Monitoring
More frequent IOP measurements can be beneficial in patients who have moderate or severe glaucoma whose disease appears to be progressing at normal IOP measurements. For these patients, glaucoma specialists want to know whether they require a very low IOP or need to limit volatility to preserve remaining visual field. These goals are entirely different when taking a surgical approach. The former requires filtering procedures to get IOP measurements down to the single digits, while the latter can benefit from less aggressive procedures that result in a “surgical mean IOP” in the low teens. For these reasons, this subset of patients likely derives the greatest benefit from remote IOP monitoring.
Other patient populations that may benefit from remote IOP monitoring include children and those who present with advanced disease. Juvenile patients with ocular hypertension are particularly challenging (Figure 1), and remote IOP monitoring could help differentiate those who have true juvenile open-angle glaucoma (JOAG).
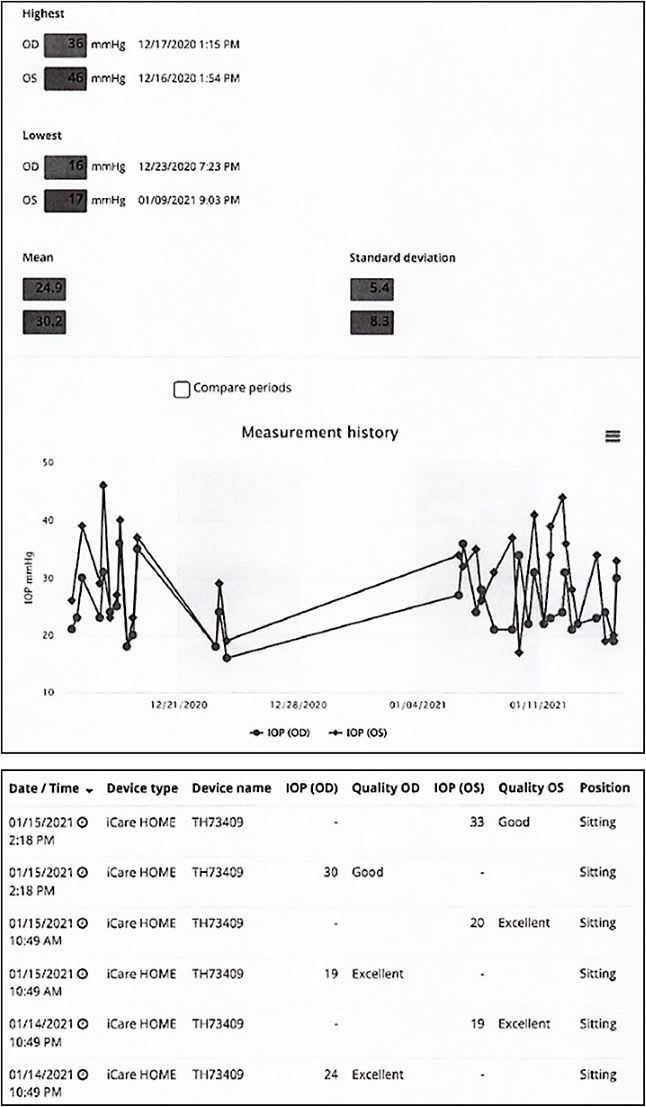
Patients with newly diagnosed advanced disease are another population where home monitoring may help guide the decision-making process. There is mounting evidence to support earlier surgical intervention for these patients. Having more data early that confirms a patient is fluctuating and not controlled may make the surgical discussion easier for both the clinician and the patient.1,2
Potential Barriers to Adoption
Although it would be beneficial in cases to have additional data on IOP fluctuation, there are practical considerations with currently available options. Patients with glaucoma have vision loss that affects their ability to use a home monitoring device, with many requiring considerable training to learn how to obtain accurate measurements. Mishandling of the devices is also an issue and this leads to challenges with having enough devices in service. The cost of these devices is not insignificant, with certain models approaching several thousand dollars each. How to bill or charge for these devices is outside the scope of this discussion.
Accuracy of IOP measurement is extremely important to glaucoma specialists. Although no method of measuring IOP is perfect, studies have shown that iCare Home is reliable, especially in patients with a normal central corneal thickness. Issues do tend to arise in measuring IOP for patients with a very thick central corneal thickness.3 The intent of home monitoring, however, is really to identify extreme outliers as opposed to slight variations in IOP.
Routine IOP Checks at Home
Remote monitoring of disease may be an area where home tonometry is useful to the comprehensive ophthalmologist and glaucoma specialist. Rather than looking for spikes in IOP, these devices can be used for routine IOP checks at home. In-office visits are vital for initial consultations and when there are changes in vision or new symptoms that are concerning. At a typical follow-up glaucoma visit, most of the exam is centered around reviewing test results and examining the optic disc for the presence of a hemorrhage. With advancing technology, doing this all from home may be a reality in the near future. Portable optical coherence tomography, virtual visual field testing, or disc photography (on a handheld device) coupled with home tonometry may significantly reduce the need for office visits. This would allow clinicians the ability to spend more time with patients who require closer attention. This will not eliminate the requirement for office visits and, of course, the results of home testing need to be reviewed in a timely manner.
Conclusion
Home monitoring of IOP has made great strides but needs to continue to improve if it is to be adopted by more providers. The technology can be difficult to use and may require a significant financial investment. Test results can be unreliable, especially if patients are not coming to the office to double-check the results. However, when coupled with other devices, home monitoring has the potential to help change the way care is delivered, as well as increase the number of patients who can be treated. This is a big need, because most glaucoma specialists would agree that patient volume is the greatest challenge they face on a daily basis. GP
References
- Levin AM, McGlumphy EJ, Chaya CJ, Wirostko BM, Johnson TV. The utility of home tonometry for peri-interventional decision-making in glaucoma surgery: Case series. Am J Ophthalmol Case Rep. 2022;28:101689. doi: 10.1016/j.ajoc.2022.101689.
- Dabasia PL, Lawrenson JG, Murdoch IE. Evaluation of a new rebound tonometer for self-measurement of intraocular pressure. Br J Ophthal. 2016; 100:1139-1143. doi: 10.1136/bjophthalmol-2015-307674.
- Mudie LI, LaBarre S, Varadaraj V, et al. The Icare HOME (TA022) study: performance of an intraocular pressure measuring device for self-tonometry by glaucoma patients. Ophthalmology. 2016;123(8):1675-1684. doi:10.1016/j.ophtha.2016.04.044










