The episcleral vascular system is a highly regulated vasculature that represents the distal portion of the conventional aqueous outflow pathway. It is a complex system of arteries, veins, and anterior venous anastomoses (AVA). Clinically, episcleral vessels are nonmobile and can be differentiated from the overlying mobile conjunctival vessels using a cotton tip. In the conventional outflow pathway, the aqueous flows from the trabecular meshwork (TM) into Schlemm’s canal (SC) and collector channels (CC) to be drained by aqueous veins and then episcleral veins.1 Episcleral venous pressure (EVP) plays a vital role in determining intraocular pressure (IOP), based on the modified Goldmann equation:
- IOP=(Q-U)/C+EVP
Q, aqueous flow rate; U, uveoscleral outflow; C, conventional outflow.
In a study including 11 subjects, Friberg et al demonstrated that for each 0.83±0.21 mmHg increase in EVP, there was a 1 mmHg increase in IOP.2 Episcleral flow rates have been estimated and observed since Ascher’s seminal work on this subject in 1949.3 Episcleral outflow provides an estimate of aqueous humor outflow and has been subjectively observed to increase after pharmacologic IOP lowering.
Because of the relationship between episcleral pressure and flow on IOP, methods that can accurately measure EVP and flow have an important role in the future of glaucoma therapy. These measures will aid in developing IOP-lowering medications and surgical interventions targeting the episcleral veins. This may open doors for personalized glaucoma management. For example, in the future, a clinician may identify a glaucoma patient with measured elevated EVP and can select a specific medication that lowers EVP. Similarly, if surgery is needed, a surgery that bypasses the conventional pathway, and hence bypasses EVP, would offer a better success rate.
Measuring Episcleral Venous Pressure and Flow
Numerous methods have been tried for EVP measurement.4 However, they are limited to being either invasive or subjective, producing variable results. Invasive techniques include either direct evaluation of EVP by cannulation of the episcleral veins or indirect evaluation by lowering the pressure in the anterior chamber (AC), allowing blood reflux into the SC and CC. The pressure that enables the reflux is presumed to correspond to the EVP.5,6
The episcleral venomanometer (EV-310; Eyetech Ltd) provides a noninvasive way to measure EVP. The device is mounted on the slit lamp in a similar fashion to the Goldmann applanation tonometer. It has a dome-shaped silicone ring on its tip, compressing episcleral veins. Pressure is gradually increased using a knob until the episcleral vein begins to blanch or collapse. The EVP is presumed to be the pressure needed when the vein collapses.7,8 Sit et al improved this method and made it more reproducible by adding a computer-controlled motor drive to increase pressure automatically, a transducer to record pressure, and a high-definition video camera to record vein collapse (Figure 1).9,10

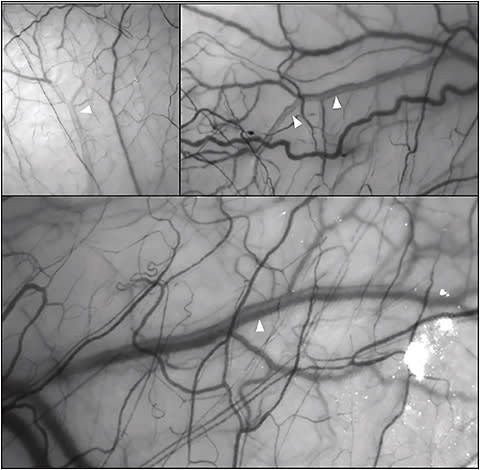
Recently, multiple methods have been developed to assess episcleral flow rates. One noninvasive method for evaluating in vivo episcleral venous flow is hemoglobin video imaging (HVI). This method assesses laminar flow within the episcleral veins. Laminar flow refers to the separation between blood and aqueous within the episcleral veins. A video camera is mounted on the slit lamp, fitted with an interference filter. When the eye is exposed to a light wavelength that corresponds to the hemoglobin absorption spectrum, the aqueous will appear as clear (being devoid of hemoglobin) within the darker hemoglobin-containing red blood cells (Figure 2). Presumably, the increased aqueous outflow will enhance the surrounding blood flow rate.11
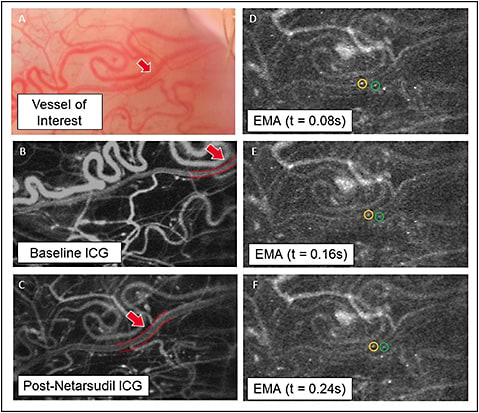
A novel method that was recently developed to measure in vivo episcleral venous flow is erythrocyte-mediated angiography (EMA).12 This technique uses autologous, indocyanine green–labelled erythrocyte “ghosts,” which are reinjected into a subject. The use of a commercially available scanning laser ophthalmoscope then permits direct visualization of erythrocytes, calculation of velocity, and episcleral flow rates (Figure 3).
Episcleral Venous Pressure in Normal and Glaucomatous Subjects
The normal range of EVP varies significantly between different studies, mainly due to different measurement methods. The reported values of EVP measured range from 7.6±1.3 mmHg to 11.4±0.2 mmHg.13,14 Several factors, such as cold air,15 pregnancy,16 and hyperthermia17 have been reported to affect EVP. Blondeau et al investigated the diurnal variations in EVP in healthy subjects using the episcleral venomanometer and reported constant EVP values except for a small reduction at night.18 Most of the published literature reported no correlation between EVP and age.19 Arora et al reported that EVP was significantly higher in the inclined position (7.8 mmHg) compared to the sitting position (6.4 mmHg), with corresponding changes in the IOP.20
Limited literature is currently available on measuring EVP in glaucoma patients compared to normal controls with conflicting results. A prospective study by Selbach et al found that the EVP was significantly higher in primary open-angle glaucoma (POAG) patients, whether high-tension glaucoma (HTG, 12.1 mmHg) or normal-tension glaucoma (NTG, 11.6 mmHg) compared to normal healthy controls (9.5 mmHg).21 On the other hand, Rickenbach and Werner reported a lower mean EVP in glaucomatous patients compared to normal controls.22 Several studies have reported no significant difference in the mean EVP between glaucoma patients and normal controls.23,24 Talusan and Schwartz reported that the EVP was significantly lower in ocular hypertension (OHT) patients compared to normal controls or POAG patients.25
Effect of Glaucoma Medications on Episcleral Venous Pressure
Several studies have shown that topical β-blockers, pilocarpine 4%, and carbonic anhydrase inhibitors do not affect EVP.26-28 The effect of prostaglandin analogues (PGAs) on EVP depends on its form (topical vs intracameral). Sponsel et al compared the effect of latanoprost and timolol-XE on EVP in healthy subjects and reported no effect of either drug on EVP.29 Another study by Toris et al conducted in OHT patients found no significant impact of unoprostone on EVP.30 Tsai et al have demonstrated that topical latanoprost may increase the EVP in normotensive dogs.7 In contrast, Lee et al evaluated the effect of intracameral bimatoprost sustained-release implants on the EVP in normotensive dogs. They demonstrated a transient increase in the EVP (peak at day 8), followed by a significant reduction compared to the baseline EVP.31
The difference in the effect of topical vs intracameral PGAs was hypothesized to be because of different actions on episcleral vasculature. Topical PGAs may induce pharmacologic vasodilation of the entire episcleral vascular system, including arteries, veins, and connecting AVA, which allows blood to flow from areas of high pressure (arteries) to areas of lower pressure (veins) through AVA, increasing the EVP. This in turn may limit further IOP-lowering effect of topical PGAs with increased dosing. On the other hand, intracameral PGAs injection causes selective dilation of the episcleral veins without affecting the arteries or the AVA, which reduces the EVP and allows for an incremental increase in the IOP-lowering effect of the drug with increasing dosing.1,32
Topical netarsudil (Rhopressa; Aerie Pharmaceuticals) is a Rho-kinase and norepinephrine transporter inhibitor. Studies have shown that its IOP-lowering effect is related to its action on increasing TM outflow and reduction of aqueous production. Additionally, there is growing evidence about its effect on reducing EVP. In a phase 2 randomized trial that included 20 patients with POAG or OHT, Sit et al showed that a once-daily dose of topical netarsudil 0.02% resulted in a significant reduction of the EVP from a baseline of 7.68±1.31 mmHg to 6.90±1.01 mmHg at day 8.33 This EVP reduction was significantly different when compared to the contralateral vehicle-treated eye. Netarsudil has also been effectively shown to have a corresponding increase in episcleral flow using EMA in a small study of 10 glaucoma suspect and OHT patients (Figure 3).34
A recent study by Suzuki et al compared the episcleral outflow of another Rho-kinase inhibitor, ripasudil (Glanatec; Kowa Ltd [approved in Japan and Korea]) to latanoprost using HVI. They reported significant dilation of the aqueous column width with ripasudil compared to latanoprost suggesting increased episcleral venous outflow.36
Effect of Selective Laser Trabeculoplasty and Glaucoma Surgery on Episcleral Venous Pressure
In a prospective study including 8 eyes that underwent selective laser trabeculoplasty (SLT), Khatib et al used HVI to demonstrate a significant increase in the aqueous column in the episcleral veins after SLT.37 Studies are under way to evaluate the episcleral venous outflow using EMA before and after different glaucoma procedures.
Bostan and Harasymowycz have proposed a grading system for episcleral laminar outflow where 0 is no laminar flow, 1 is faint laminar flow, and 2 is marked laminar flow. They retrospectively evaluated patients who underwent iStent (Glaukos) surgery and correlated between the postoperative IOP and glaucoma medications and the laminar flow in the episcleral vein closest to the iStent implantation. They reported a significantly lower postoperative IOP and number of medications in patients with 2+ laminar flow compared to those with 0 laminar flow. However, the difference was not significant when comparing patients with 1+ laminar flow to those with 0 laminar flow.38
Conclusion
Measurement of EVP and episcleral venous flow offers a potential future of personalized medicine in glaucoma management. Future advances may enable ophthalmologists to determine areas of reduced EVP and reduced episcleral venous flow preoperatively, permitting more focused and targeted minimally invasive glaucoma surgeries and ultimately improving surgical outcomes and success rates. GP
References
- Lee SS, Robinson MR, Weinreb RN. Episcleral venous pressure and the ocular hypotensive effects of topical and intracameral prostaglandin analogs. J Glaucoma. 2019;28(9):846-857. doi:10.1097/ijg.0000000000001307
- Friberg TR, Sanborn G, Weinreb RN. Intraocular and episcleral venous pressure increase during inverted posture. Am J Ophthalmol. 1987;103(4):523-526. doi:10.1016/s0002-9394(14)74275-8
- Ascher KW. Aqueous veins and their significance for pathogenesis of glaucoma. Arch Ophthal. 1949;42(1):66-76. doi: 10.1001/archopht.1949.00900050069006
- Sit AJ, McLaren JW. Measurement of episcleral venous pressure. Exp Eye Res. 2011;93(3):291-298. doi:10.1016/j.exer.2011.05.003
- Aihara M, Lindsey JD, Weinreb RN. Episcleral venous pressure of mouse eye and effect of body position. Curr Eye Res. 2003;27(6):355-362. doi:10.1076/ceyr.27.6.355.18194
- Greenwood M, Berdahl J, Ibach M. New technology and current understanding of episcleral venous pressure. Curr Ophthal Rep. 2018;6(2):86-92. doi:10.1007/s40135-018-0168-1
- Tsai S, Miller PE, Struble C, et al. Topical application of 0.005% latanoprost increases episcleral venous pressure in normal dogs. Vet Ophthalmol. 2012;15 Suppl 1:71-78. doi:10.1111/j.1463-5224.2011.00970.x
- Arora N, McLaren JW, Sit AJ. Variations of episcleral venous pressure with body position in healthy subjects. Invest Ophthalmol Vis Sci. 2012;53(3):1988.
- Kazemi A, McLaren JW, Sit AJ. Effect of topical phenylephrine 2.5% on episcleral venous pressure in normal human eyes. Invest Ophthalmol Vis Sci. 2021;62(10):4. doi:10.1167/iovs.62.13.4
- Sit AJ, Ekdawi NS, Malihi M, McLaren JW. A novel method for computerized measurement of episcleral venous pressure in humans. Exp Eye Res. 2011;92(6):537-544. doi:10.1016/j.exer.2011.03.018
- Meyer PAR. Re-orchestration of blood flow by micro-circulations. Eye. 2018;32(2):222-229. doi:10.1038/eye.2017.315
- Asanad S, Park A, Pottenburgh J, Siddiqui A, Mayo L, Saeedi OJ. Erythrocyte-mediated angiography: quantifying absolute episcleral blood flow in humans. Ophthalmology 2021;128(5):799-801. doi:10.1016/j.ophtha.2020.09.010
- Linner E, Rickenbach C, Werner H. Comparative measurements of the pressure in the aqueous veins and the conjunctival veins using different methods. Acta Ophthalmol (Copenh). 1950;28(4):469-478. doi:10.1111/j.1755-3768.1950.tb00002.x
- Zeimer RC, Gieser DK, Wilensky JT, Noth JM, Mori MM, Odunukwe EE. A practical venomanometer. Measurement of episcleral venous pressure and assessment of the normal range. Arch Ophthalmol. 1983;101(9):1447-1449. doi:10.1001/archopht.1983.01040020449024
- Ortiz GJ, Cook DJ, Yablonski ME, Masonson H, Harmon G. Effect of cold air on aqueous humor dynamics in humans. Invest Ophthalmol Vis Sci. 1988;29(1):138-140.
- Wilke K. Episcleral venous pressure and pregnancy [proceedings]. Acta Ophthalmol Suppl. 1975(125):40-41. doi:10.1111/j.1755-3768.1975.tb01228.x
- Krupin T, Bass J, Oestrich C, Podos SM, Becker B. The effect of hyperthermia on aqueous humor dynamics in rabbits. Am J Ophthalmol. 1977;83(4):561-564. doi:10.1016/0002-9394(77)90567-0
- Blondeau P, Tétrault J-P, Papamarkakis C. Diurnal variation of episcleral venous pressure in healthy patients: a pilot study. J Glaucoma. 2001;10(1):18-24. doi:10.1097/00061198-200102000-0000
- Gaasterland D, Kupfer C, Milton R, Ross K, McCain L, MacLellan H. Studies of aqueous humour dynamics in man. VI. Effect of age upon parameters of intraocular pressure in normal human eyes. Exp Eye Res. 1978;26(6):651-656. doi:10.1016/0014-4835(78)90099-4
- Arora N, McLaren JW, Hodge DO, Sit AJ. Effect of body position on epsicleral venous pressure in healthy subjects. Invest Ophthalmol Vis Sci. 2017;58(12):5151-5156. doi:10.1167/iovs.17-22154
- Selbach JM, Posielek K, Steuhl KP, Kremmer S. Episcleral venous pressure in untreated primary open-angle and normal-tension glaucoma. Ophthalmologica. 2005;219(6):357-361. doi:10.1159/000088378
- Rickenbach K, Werner H. Scheinbarer abflußdruck, tension und druck in kammerwasservenen. Ophthalmologica. 1950;120(1-2):22-27. doi:10.1159/000300857
- Leith AB. Episcleral venous pressure in tonography. Br J Ophthalmol. 1963;47(5):271. doi:10.1136/bjo.47.5.271
- Podos SM, Minas TF, Macri FJ. A new instrument to measure episcleral venous pressure: comparison of normal eyes and eyes with primary open-angle glaucoma. Arch Ophthalmol. 1968;80(2):209-213. doi:10.1001/archopht.1968.00980050211011
- Talusan ED, Schwartz B. Episcleral venous pressure: differences between normal, ocular hypertensive, and primary open-angle glaucomas. Arch Ophthalmol. 1981;99(5):824-828. doi:10.1001/archopht.1981.03930010824006
- Schenker HI, Yablonski ME, Podos SM, Linder L. Fluorophotometric study of epinephrine and timolol in human subjects. Arch Ophthalmol. 1981;99(7):1212-1216. doi:10.1001/archopht.1981.03930020086007
- Yablonski ME, Zimmerman TJ, Waltman SR, Becker B. A fluorophotometric study of the effect of topical timolol on aqueous humor dynamics. Exp Eye Res. 1978;27(2):135-142. doi:10.1016/0014-4835(78)90083-0
- Yablonski ME, Novack GD, Burke PJ, Cook DJ, Harmon G. The effect of levobunolol on aqueous humor dynamics. Exp Eye Res. 1987;44(1):49-54. doi:10.1016/s0014-4835(87)80024-6
- Sponsel WE, Mensah J, Kiel JW, et al. Effects of latanoprost and timolol-XE on hydrodynamics in the normal eye. Am J Ophthalmol. 2000;130(2):151-159. doi:10.1016/s0002-9394(00)00401-3
- Toris CB, Zhan G, Camras CB. Increase in outflow facility with unoprostone treatment in ocular hypertensive patients. Arch Ophthalmol. 2004;122(12):1782-1787. doi:10.1001/archopht.122.12.1782
- Lee SS, Burke J, Shen J, et al. Bimatoprost sustained-release intracameral implant reduces episcleral venous pressure in dogs. Vet Ophthalmol. 2018;21(4):376-381. doi:10.1111/vop.12522
- Lee SS, Dibas M, Almazan A, Robinson MR. Dose-response of intracameral bimatoprost sustained-release implant and topical bimatoprost in lowering intraocular pressure. J Ocul Pharmacol Ther. 2019;35(3):138-144. doi:10.1089/jop.2018.0095
- Sit AJ, Gupta D, Kazemi A, et al. Netarsudil improves trabecular outflow facility in patients with primary open-angle glaucoma or ocular hypertension: a phase 2 study. Am J Ophthalmol. 2021;226:262-269. doi:https://doi.org/10.1016/j.ajo.2021.01.019
- Kim S, Chen V, Cruz M, Pottenburgh J, Saeedi OJ. Precise quantification of episcleral venous flow rates in human subjects before and after netarsudil 0.02%. Invest Ophthalmol Vis Sci. 2022;63(7):3497.
- Saeedi OJ. Single-cell erythrocyte tracking in human subjects reveals increase in episcleral venous flow with netarsudil 0.02%. Presented at: annual meeting of the American Academy of Ophthalmology; September 30-October 3, 2022; Chicago, IL.
- Suzuki M, Suzuki Y, Komori R, et al. Aqueous column changes in the episcleral veins after the instillation of ripasudil versus latanoprost: a randomized, double-blind, crossover clinical trial. Sci Rep. 2022;12(1):15255. doi:10.1038/s41598-022-19271-9
- Khatib TZ, Meyer PAR, Lusthaus J, Manyakin I, Mushtaq Y, Martin KR. Hemoglobin video imaging provides novel in vivo high-resolution imaging and quantification of human aqueous outflow in patients with glaucoma. Ophthalmol Glaucoma. 2019;2(5):327-335. doi:10.1016/j.ogla.2019.04.001
- Bostan C, Harasymowycz P. Episcleral venous outflow: a potential outcome marker for iStent surgery. J Glaucoma. 2017;26(12):1114-1119. doi:10.1097/IJG.0000000000000799