Glaucoma is a heterogeneous group of diseases characterized by morphologic damage to the optic nerve head (ONH) and attendant visual field loss localizing to the nerve fiber layer territory. It is a leading cause of blindness worldwide, and predictions estimate that more than 110 million people will be affected by 2040.1 Primary open-angle glaucoma (POAG) is the most common form where optic nerve damage occurs in the context of increased intraocular pressure (IOP) compared to uninvolved subjects and the gonioscopic appearance of an open filtration angle. This article will describe important genetic biomarkers associated with clinically important glaucoma phenotypes and POAG, including corneal hysteresis (CH), IOP, cup-to-disc ratio (CDR), and central cornea thickness (CCT).
Corneal Hysteresis
The term hysteresis refers to the bend-but-not-break mentality associated with resilience. From an engineering perspective, hysteresis represents the difference between how a material deforms and reforms during loading and unloading from an applied force. Corneal hysteresis is measured in millimeters of mercury (mmHg) after the application of an air bolus sufficient to indent the cornea. It is a highly heritable trait, and a typical 60-year-old person will have a CH value of a little over 10 mmHg.2 Corneal hysteresis decreases with age, and a lower CH has previously been shown to be associated with an increased risk of glaucoma progression,3-4 making this biomarker one of emerging clinical importance. The top genetic biomarkers associated with CH are COL6A1, COL6A2, and COL6A3, which encode for the various components of collagen type VI,5 which makes up ~25% of the cornea’s dry weight.6 Furthermore, collagen type VI colocalizes with myocilin in the trabecular meshwork.7
Intraocular Pressure
Intraocular pressure is the only modifiable risk factor for POAG. There is strong shared heritability between IOP and POAG, meaning that many gene variants related to higher IOP are also related to increased risk of POAG.8 More than 100 common gene variants have been identified for IOP.9 Genetic loci in the MYOC gene, which codes for myocilin, are the most uncommon of these variants (mean allele frequency <0.3%) but they have the highest effect size (~almost 3 mmHg per risk allele).10 Of the common IOP gene variants (those with mean allele frequency >10%), TMCO1, which codes for transmembrane and coiled-coil domain 1, has the largest positive impact on IOP (~0.4 mmHg per risk allele). While this effect size seems small, a TMCO1 allele associated with higher IOP was an independent determinant of the conversion from ocular hypertension to POAG in the Ocular Hypertension Treatment Study.11 While TMCO1 plays an essential role in maintaining Ca (2+) homeostasis within the endoplasmic reticulum,12 its role in modulating IOP levels is not entirely clear.
Can any discovered IOP genetic biomarkers be targeted to treat glaucoma? MYOC is a small gene with 3 exons — all the IOP-increasing gene variants are in the last exon and produce gain-of-protein function. There is evidence that a gene-editing approach that knocks down myocilin expression produces lower IOP in a murine glaucoma model.13 If this gene-editing approach is translated to humans, perhaps with a minimally invasive glaucoma surgery approach, it may benefit patients with the exon 3 mutation in MYOC.
Another promising therapeutic target is ANGPT7, which codes for angiopoietin 7, a protein strongly expressed in the human trabecular meshwork.14 Angiopoietin 7 increases trabecular meshwork resistance, especially in the face of high corticosteroid levels. Interestingly, a rare loss-of-function coding variant in ANGPT7 was associated with lower IOP. ANGPT7 knock-out mice have a 2 mmHg lower IOP compared to wild-type mice. Genetic silencing of ANGPT7 may ultimately have widespread utility in human open-angle glaucoma.
Cup-to-Disc Ratio
A larger CDR is an IOP-independent risk factor for the conversion from OHTN to POAG.15 When an artificial intelligence algorithm was applied to ascertain disc-diameter adjusted vertical cup-to-disc ratio in 3 large data repositories of fundus images linked to high throughput genotyping data, more than 200 genetic variants were associated with CDR, chief among them being CDKN2B-AS.16 Nearly 30% of these variants were also associated with POAG after adjusting for multiple comparisons. CDKN2B-AS variants related to CDR seem to modify optic nerve vulnerability in POAG. The POAG patients in 2 US-based consortia with at least one A allele at a CDKN2B-AS locus associated with increased risk of POAG (rs3217992) had larger CDR despite having lower IOP at DNA collection as compared to patients with wild-type alleles at this locus.17 CDKN2B-AS codes for a long noncoding RNA, which may have a role in cell cycling as evidenced by studies showing variants in this region associated with tumorigenicity18 and chemotherapy resistance.19 Perhaps CDKN2B-AS contributes to the pathobiology of glaucoma by exerting its effects on reactive microglia that support retinal ganglion cells.
Central Corneal Thickness
Central corneal thickness is amongst the most highly heritable traits in medicine (95% heritable).20 Most recent genome-wide studies suggest that there are over 200 loci related to CCT. Lower CCT is a risk factor for the conversion from ocular hypertension to POAG,20 but it is unclear if it is a risk factor for POAG in populations where the preponderance of IOPs is much lower than those required for entry criteria into the Ocular Hypertension Treatment Study (≥24 mmHg in one eye and ≥22 mmHg in the fellow eye).
Interestingly, there is minimal, if any, shared heritability between loci associated with CCT and loci associated with POAG.21 Rather, 24 out of 233 CCT loci (10%) are associated with keratoconus. The top common variant associated with thinner CCT is ZNF469 and a rare variant in this variant is responsible for a Mendelian variant of corneal ectasia called brittle corneal syndrome, where CCT can drop below 300 µm, leading to spontaneous corneal perforation.22 On the other hand, ZNF469 variants are not associated with POAG.
Exploring Multiple Pathways
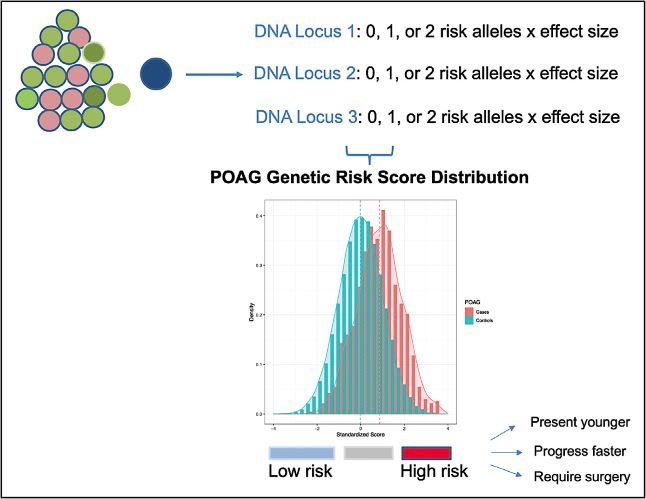
Primary open-angle glaucoma is a prototypical complex polygenetic disease in that every time the sample size doubles, the number of genetic loci associated with the condition doubles. The most recent large-scale genome-wide association study, consisting of 34,179 cases and 349,321 controls, reported 127 POAG-related loci.23 As the genetic architecture for POAG suggests that multiple pathophysiologic mechanisms may be implicated in any given patient, there is a move to explore the clinical utility of genetic risk scores that combine the blended effect of all these mechanisms. Patients with higher genetic risk scores for POAG have earlier onset disease, are more likely to present with more significant functional loss, and are more likely to require invasive surgery.24 As we learn more about the utility of POAG polygenetic risk scores, these scores may play a role in future glaucoma screening strategies, disease prediction, and precision medicine approach for POAG (Figure 1).
Not surprisingly, because POAG is a complex disease, the discovered loci point to a myriad of processes in the disease including endothelial cell function, immune mechanisms, mitochondrial biogenesis, extracellular matrix alterations, and multiple biochemical pathways like lipid and glucose metabolism.23 This indicates that multiple drug targets for POAG may emerge, but precision medicine approaches to treatment may require a multi-prong approach depending on a patient’s aggregate genetic risk to POAG. One FDA-approved drug that emerges as a potential glaucoma treatment based on analysis of the latest POAG genes is dipyridamole, which is a 3’,5’-cyclic phosphodiesterase inhibitor that may improve blood flow in the glaucomatous optic nerve.23 Since the unmyelinated segment of the optic nerve has a high density of mitochondria, and since several gene variants point to genes involved in mitochondrial energy production, it is reasonable to target NAD+/NADH redox state as a potential therapeutic target in glaucoma. There are promising preclinical and clinical data to support the performance of a randomized clinical trial to assess nicotinamide supplementation in the treatment of glaucoma.25-26
Summary
The study of genetic biomarkers and glaucoma will continue to encompass larger datasets that will fill in the genetic architecture for this disease and its related endophenotypes. Furthermore, technological advances in metabolomics and proteomics will allow for high throughput searches of downstream biomarkers that reflect the interactions of genes and environment in glaucoma. For example, aptamer-based technologies that use single-stranded DNA-like antibodies to bind, allowing for the simultaneous assessment and quantification of 7,000 proteins.27 The merger of these data sets with imaging and electronic medical record repositories will create a multiomic framework that will facilitate understanding of the variable IOP levels and optic nerve vulnerabilities on an individual patient level.
The genetics of glaucoma, as it pertains to several endophenotypes and biomarkers, is a new frontier for the diagnosis and management of glaucoma. Future studies will enable treatment modalities beyond the current paradigm. Other biomarkers will continue to emerge from further research into metabolomics, proteomics, and the microbiome. GP
References
- Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121(11):2081-2090. doi:10.1016/j.ophtha.2014.05.013.
- Carbonaro F, Andrew T, Mackey DA, Spector TD, Hammond CJ. The heritability of corneal hysteresis and ocular pulse amplitude: a twin study. Ophthalmology. 2008;115(9):1545-1549. doi:10.1016/j.ophtha.2008.02.011
- Celebi ARC, Kilavuzoglu AE, Altiparmak UE, Cosar Yurteri CB. Age-related change in corneal biomechanical parameters in a healthy Caucasian population. Ophthalmic Epidemiol. 2018;25(1):55-62. doi:10.1080/09286586.2017.1351997
- Jammal AA, Medeiros FA. Corneal hysteresis and rates of neuroretinal rim change in glaucoma. Ophthalmol Glaucoma. 2022;5(5):483-489. doi:10.1016/j.ogla.2022.03.006
- Simcoe MJ, Khawaja AP, Hysi PG, Hammond CJ; UK Biobank Eye and Vision Consortium. Genome-wide association study of corneal biomechanical properties identifies over 200 loci providing insight into the genetic etiology of ocular diseases. Hum Mol Genet. 2020;29(18):3154-3164. doi:10.1093/hmg/ddaa155
- Zimmermann DR, Trüeb B, Winterhalter KH, Witmer R, Fischer RW. Type VI collagen is a major component of the human cornea. FEBS Lett. 1986;197(1-2):55-58. doi:10.1016/0014-5793(86)80297-6
- Tawara A, Okada Y, Kubota T, et al. Immunohistochemical localization of MYOC/TIGR protein in the trabecular tissue of normal and glaucomatous eyes. Curr Eye Res. 2000;21(6):934-943. doi:10.1076/ceyr.21.6.934.6988.
- Aschard H, Kang JH, Iglesias AI, et al. Genetic correlations between intraocular pressure, blood pressure and primary open-angle glaucoma: a multi-cohort analysis. Eur J Hum Genet. 2017;25(11):1261-1267. doi:10.1038/ejhg.2017.136
- Khawaja AP, Cooke Bailey JN, Wareham NJ, et al. Genome-wide analyses identify 68 new loci associated with intraocular pressure and improve risk prediction for primary open-angle glaucoma. Nat Genet. 2018;50(6):778-782. doi:10.1038/s41588-018-0126-8.
- Xu Z, Hysi P, Khawaja AP. Genetic determinants of intraocular pressure. Annu Rev Vis Sci. 2021;7:727-746. doi:10.1146/annurev-vision-031021-095225
- Scheetz TE, Faga B, Ortega L, et al. Glaucoma risk alleles in the Ocular Hypertension Treatment Study. Ophthalmology. 2016;123(12):2527-2536. doi:10.1016/j.ophtha.2016.08.036
- Yang KY, Zhao S, Feng H, et al. Ca2+ homeostasis maintained by TMCO1 underlies corpus callosum development via ERK signaling. Cell Death Dis. 2022;13(8):674. doi:10.1038/s41419-022-05131-x
- Jain A, Zode G, Kasetti RB, et al. CRISPR-Cas9–based treatment of myocilin-associated glaucoma. Proc Natl Acad Sci U S A. 2017;114(42):11199-11204. doi:10.1073/pnas.1706193114
- Praveen K, Patel GC, Gurski L, et al. ANGPTL7, a therapeutic target for increased intraocular pressure and glaucoma. Commun Biol. 2022;5(1):1051. doi:10.1038/s42003-022-03932-6
- Gordon MO, Beiser JA, Brandt JD, et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):714-720. doi:10.1001/archopht.120.6.714
- Han X, Steven K, Qassim A, et al. Automated AI labeling of optic nerve head enables insights into cross-ancestry glaucoma risk and genetic discovery in >280,000 images from UKB and CLSA. Am J Hum Genet. 2021;108(7):1204-1216. doi:10.1016/j.ajhg.2021.05.005
- Pasquale LR, Loomis SJ, Kang JH, et al. CDKN2B-AS1 genotype-glaucoma feature correlations in primary open-angle glaucoma patients from the United States. Am J Ophthalmol. 2013;155(2):342-353.e5. doi:10.1016/j.ajo.2012.07.023
- Deng W, Zhang Y, Cai J, et al. LncRNA-ANRIL promotes gastric cancer progression by enhancing NF-kB signaling. Exp Biol Med (Maywood). 2019;244(12):953-959. doi:10.1177/1535370219860207
- Shang C, Ao CN, Cheong CC, Meng L. Long non-coding RNA CDKN2B antisense RNA 1 gene contributes to paclitaxel resistance in endometrial carcinoma. Front Oncol. 2019;29(9):27. doi:10.3389/fonc.2019.00027
- Toh T, Liew SH, MacKinnon JR, et al. Central corneal thickness is highly heritable: the twin eye studies. Invest Ophthalmol Vis Sci. 2005;46(10):3718-3722. doi:10.1167/iovs.04-1497
- He W, Han X, Ong JS, et al. Association of novel loci with keratoconus susceptibility in a multitrait genome-wide association study of the UK Biobank Database and Canadian Longitudinal Study on Aging. JAMA Ophthalmol. 2022;140(6):568-576. doi:10.1001/jamaophthalmol.2022.0891
- Lu Y, Dimasi DP, Hysi PG, et al. Common genetic variants near the Brittle Cornea Syndrome locus ZNF469 influence the blinding disease risk factor central corneal thickness. PLoS Genet. 2010;6(5):e1000947. doi:10.1371/journal.pgen.1000947
- Gharahkhani P, Jorgenson E, Hysi P, et al. Genome-wide meta-analysis identifies 127 open-angle glaucoma loci with consistent effect across ancestries. Nat Commun. 2021;12(1):1258. doi:10.1038/s41467-020-20851-4
- Craig JE, Han X, Qassim A, et al. Multitrait analysis of glaucoma identifies new risk loci and enables polygenic prediction of disease susceptibility and progression. Nat Genet. 2020; 52(2):160-166. doi:10.1038/s41588-019-0556-y
- Zhang X, Zhang N, Chrenek MA, et al. Systemic treatment with nicotinamide riboside is protective in 2 mouse models of retinal ganglion cell damage. Pharmaceutics. 2021;13(6):893. doi:10.3390/pharmaceutics13060893
- De Moraes CG, John SWM, Williams PA, Blumberg DM, Cioffi GA, Liebmann JM. Nicotinamide and pyruvate for neuroenhancement in open-angle glaucoma: a phase 2 randomized clinical trial. JAMA Ophthalmol. 2022;140(1):11-18. doi:10.1001/jamaophthalmol.2021.4576
- Pietzner M, Wheeler E, Carrasco-Zanini J, et al. Synergistic insights into human health from aptamer- and antibody-based proteomic profiling. Nat Commun. 2021;12(1):6822. doi:10.1038/s41467-021-27164-0










