Glaucoma is a leading cause of irreversible blindness, and current approaches to treatment are focused on decreasing intraocular pressure (IOP), the only modifiable risk factor associated with disease progression.1,2 The treatment of glaucoma has undergone major advancement over the last decade, with emergence of new medical and surgical options.3,4 Further, the approach to treatment has shifted with recently published data providing insight to shape the treatment algorithm of clinicians.5 Overall, the growth and evolution has enabled clinicians to provide a more individualized approach to treatment for patients with glaucoma.
For the surgical management of glaucoma, the risks associated with traditional glaucoma procedures such as trabeculectomy and tube shunt procedures are well established, which prompted the development of minimally invasive glaucoma surgery (MIGS).4 The MIGS space continues to grow and evolve, and the addition of MIGS has stimulated a more proactive, interventional approach in the treatment of glaucoma. Nonetheless, these procedures still carry the risks associated with intraocular surgery. Moreover, many patients do not achieve an adequate reduction in IOP and demonstrate progression of disease despite having an apparent “controlled” IOP value.6 This is particularly true in patients with normal-tension glaucoma and severe open-angle glaucoma, 2 subsets of glaucoma in which the current range of treatments such as lasers, medications, and MIGS procedures have diminished efficacy. Thus, clinicians and patients remain interested in nonsurgical treatment options for glaucoma. Several noninvasive options have recently been introduced, and recent research has shed light on potential benefits of oral supplementation. This article will provide an overview of current and future nonsurgical treatment options.
Negative Pressure Goggles
For noninvasive and nonsurgical treatments, there are several exciting options currently in development with promising early data. The Multi-Pressure Dial negative pressure goggles (Equinox Ophthalmic) consist of a programmable, pressure-modulating pump connected to a pair of specialized, pressure-sensing goggles.7,8 When the goggles are worn by a patient, the device applies negative pressure (or vacuum) to create a localized decrease in atmospheric pressure contacting the surface of the eye, leading to a decrease in IOP. The data evaluating the device thus far is impressive with an excellent safety profile and multiple studies highlighting the IOP-lowering efficacy of the device, including a recently published clinical trial.7
Optogenetics
Optogenetics is a relatively new technology that employs light to modify the cellular activity of targeted cells.9 The use of optogenetics in diseases like glaucoma is focused on regeneration of dysfunctional or lost photoreceptors by introducing light-sensitive proteins into retinal neurons. This offers a unique strategy of targeting patients with sustained vision loss that may solely rely on low-vision rehabilitation to accomplish daily tasks. Preliminary studies demonstrated successful reactivation of previously light-insensitive retinas using this technology in animal models. Optogenetics differs from gene therapy in that optogenetics is able to target neurons not only in the “vertical” visual pathway (photoreceptors, bipolar cells, and retinal ganglion cells) but also the “horizontal” visual pathway (amacrine and horizontal cells). Although optogenetics has largely been studied in animal models with retinal dystrophies, the ability for optogenetics to protect the inner retina is of major interest and currently being researched for its utility in glaucoma.10
Novel Medical Therapies
QLS-101 (Qlaris Bio) is an emerging IOP-lowering drop that employs a unique and novel mechanism of action for IOP reduction.11 The mechanism of action works to enhance outflow through the widening of outflow channels and episcleral vessels by acting as an adenosine triphosphate (ATP)-sensitive potassium channel modulator. As an EVP-lowering agent, this agent has unique appeal, as it could be an option for patients with IOPs in the low teens who need additional IOP reduction but are not great candidates for surgical treatment.11 Further, it could be an exciting option for patients with normal-tension glaucoma, a subtype of glaucoma that historically has been difficult to treat with noninvasive treatment options. This agent is currently in active clinical trials, but data thus far have been promising, with early reports suggesting favorable IOP lowering and minimal side effects including minimal conjunctival hyperemia, a common side effect in drugs targeting EVP.
Drug-eluting Technology
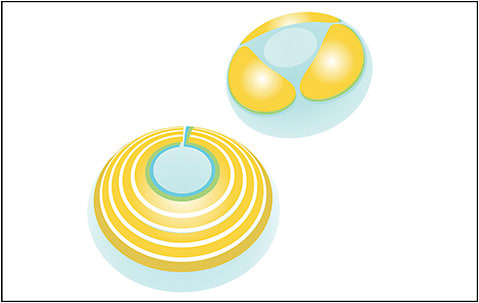
There has been notable recent innovation related to drug delivery for glaucoma, such as drug-eluting contact lenses that are in development using a proprietary printing technology (MediPrint Ophthalmics) (Figure 1). The contact lens (LL-BMT1) is printed with bimatoprost to provide an IOP-lowering effect and represents a completely novel approach to treatment of glaucoma. Interim analysis from the ongoing phase 2 study (SIGHT-2) reported favorable IOP-lowering and safety results but the study is ongoing.
Neuroprotective Strategies
In addition to new IOP-lowering treatment options, there has also been much research dedicated to the IOP-independent mechanisms that may contribute to glaucomatous damage.12 This has led to an interest in neuroprotective strategies, and multiple therapies have been proposed and are currently being investigated including dietary supplementation, cell and gene-based therapies, and neurotrophic factors.13,14 For dietary supplementation, a number of different options, primarily antioxidants, have been studied for a potential benefit in glaucoma. It has long been postulated that mitochondrial dysfunction plays an important role in the development of glaucoma, and this has been supported by animal models.15 Further, work has shown that nicotinamide adenine dinucleotide (NAD, an essential component of mitochondrial vitality) declines as we age and may contribute to susceptibility of retinal ganglion cells. This has led to an interest in NAD supplementation as a potential adjunctive treatment option for glaucoma.16,17
A recently published cross-sectional study in Journal of Glaucoma explored the association between niacin (which the body converts to NAD) intake and glaucoma across a 3-year period.18 Results of this study suggested a possible protective effect of niacin, with higher levels of niacin being associated with decreasing odds of glaucoma overall. In addition, a small clinical trial evaluating the use of supplemental nicotinamide (also a precursor to NAD) combined with pyruvate reported a short-term improvement in visual function.19 In this prospective, randomized study, 21 patients with moderate POAG were started on daily NAD in combination with pyruvate and results demonstrated a short-term improvement in visual function based on visual field testing.19 The adjunctive use of pyruvate in combination with NAD was driven by studies showing that the combination is more effective than each nutrient alone. While further study is needed and is likely under way, these promising results should promote development of novel agents supporting the health of mitochondria to combat glaucomatous damage.
In addition to oral supplementation, there has also been research exploring the use of neuroprotective agents in a topical formulation. Over the last decade, a number of studies have evaluated the use of topical citicoline as a neuroprotective agent in the treatment of glaucoma, and a recent randomized, controlled trial evaluated the use of topical citicoline over 3 years in glaucoma patients.20 In this study, patients exhibiting disease progression despite a “controlled” IOP value were treated with topical citicoline as an adjuvant treatment option, and the study reported favorable results. Although the study acknowledged multiple limitations, the results were suggestive of topical citicoline as a potential complementary treatment option.
Conclusion
The underlying mechanisms driving glaucomatous damage are likely multifactorial in nature, and this has prompted the interest and development of treatment options that aim to treat the neurodegeneration of glaucoma beyond lowering of IOP. Although negative pressure goggles and emerging medical therapies are exciting options for safely reducing IOP, this article summarizes a number of treatment options that target IOP-independent pathways to slow or halt disease progression in glaucoma. Continued innovation for the treatment of glaucoma is needed, as it remains a difficult disease to treat and a leading cause of global blindness. GP
References
- Heijl A, Leske MC, Bengtsson B, et al. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002;120(10):1268-1279. doi:10.1001/archopht.120.10.1268
- Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121(11):2081-2090. doi:10.1016/j.ophtha.2014.05.013
- Conlon R, Saheb H, Ahmed IIK. Glaucoma treatment trends: a review. Can J Ophth. 2017;52(1):114-124. doi:10.1016/j.jcjo.2016.07.013
- Shah M. Micro-invasive glaucoma surgery - an interventional glaucoma revolution. Eye Vis (Lond). 2019;6:29. doi:10.1186/s40662-019-0154-1
- Garg A, Vickerstaff V, Nathwani N, et al. Primary selective laser trabeculoplasty for open-angle glaucoma and ocular hypertension: clinical outcomes, predictors of success, and safety from the Laser in Glaucoma and Ocular Hypertension Trial. Ophthalmology. 2019;126(9):1238-1248. doi:10.1016/j.ophtha.2019.04.012
- Leske MC, Heijl A, Hussein M, Bengtsson B, Hyman L, Komaroff E. Factors for glaucoma progression and the effect of treatment: the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2003;121(1):48-56. doi:10.1001/archopht.121.1.48
- Samuelson TW, Ferguson TJ, Brubaker JW, et al. Negative pressure application via a multi-pressure dial to lower IOP in patients with suspected glaucoma or open-angle glaucoma. J Glaucoma. 2023;10.1097/IJG.0000000000002231. doi:10.1097/IJG.0000000000002231
- Swan RJ, Ferguson TJ, Shah M, et al. Evaluation of the IOP-lowering effect of a multi-pressure dial at different negative pressure settings. Trans Vis Sci Tech. 2020;9(12). doi:https://doi.org/10.1167/tvst.9.12.19
- Prosseda PP, Tran M, Kowal T, Wang B, Sun Y. Advances in ophthalmic optogenetics: approaches and applications. Biomolecules. 2022;12(2):269. doi:10.3390/biom12020269
- Kowal TJ, Prosseda PP, Ning K, et al. Optogenetic modulation of intraocular pressure in a glucocorticoid-induced ocular hypertension mouse model. Transl Vis Sci Technol. 2021;10(6):10. doi:10.1167/tvst.10.6.10
- Pervan-Steel CL, Roy Chowdhury U, Sookdeo HK, et al. Ocular hypotensive properties and biochemical profile of QLS-101, a novel ATP-sensitive potassium (KATP) channel opening prodrug. Invest Ophthalmol Vis Sci. 2022;63(4):26. doi:10.1167/iovs.63.4.26
- Susanna R Jr, De Moraes CG, Cioffi GA, Ritch R. Why do people (still) go blind from glaucoma?. Transl Vis Sci Technol. 2015;4(2):1. doi:10.1167/tvst.4.2.1
- Guymer C, Wood JP, Chidlow G, Casson RJ. Neuroprotection in glaucoma: recent advances and clinical translation. Clin Exp Ophthalmol. 2019;47(1):88-105. doi:10.1111/ceo.13336
- Chang EE, Goldberg JL. Glaucoma 2.0: neuroprotection, neuroregeneration, neuroenhancement. Ophthalmology. 2012;119(5):979-986. doi:10.1016/j.ophtha.2011.11.003
- Williams PA, Harder JM, Foxworth NE, et al. Vitamin B3 modulates mitochondrial vulnerability and prevents glaucoma in aged mice. Science. 2017;355(6326):756-760. doi:10.1126/science.aal0092
- Hui F, Tang J, Williams PA, et al. Improvement in inner retinal function in glaucoma with nicotinamide (vitamin B3) supplementation: a crossover randomized clinical trial. Clin Exp Ophthalmol. 2020;48(7):903-914. doi:10.1111/ceo.13818
- Goulart Nacácio E Silva S, Occhiutto ML, Costa VP. The use of nicotinamide and nicotinamide riboside as an adjunct therapy in the treatment of glaucoma. Eur J Ophthalmol. 2023;11206721231161101. doi:10.1177/11206721231161101
- Lee SY, Tseng VL, Kitayama K, et al. Associations between niacin intake and glaucoma in the National Health and Nutrition Examination Survey. J Glaucoma. 2023;32(6):443-450. doi:10.1097/IJG.0000000000002216
- De Moraes CG, John SWM, Williams PA, Blumberg DM, Cioffi GA, Liebmann JM. Nicotinamide and pyruvate for neuroenhancement in open-angle glaucoma: a phase 2 randomized clinical trial. JAMA Ophthalmol. 2022;140(1):11-18. doi:10.1001/jamaophthalmol.2021.4576
- Rossetti L, Iester M, Tranchina L, et al. Can treatment with citicoline eyedrops reduce progression in glaucoma? the results of a randomized placebo-controlled clinical trial. J Glaucoma. 2020;29(7):513-520. doi:10.1097/IJG.0000000000001565









